Abstract
BACKGROUND AND AIMS: In this study, a prevalence survey of various atherosclerosis risk factors was carried out on hitherto poorly studied rural–urban migrants settled in urban slums in a large metropolitan city in northern India, with the aim of studying anthropometric and metabolic characteristics of this population in socio-economic transition.
DESIGN: A cross-sectional epidemiological descriptive study.
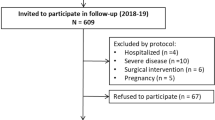
SUBJECTS: A total of 532 subjects (170 males and 362 females) were included in the study (response rate approximately 40%).
METHODS AND RESULTS: In this study, diabetes mellitus was recorded in 11.2% (95% CI 6.8–16.9) of males and 9.9% (95% CI 7.0–13.5) of females, the overall prevalence being 10.3% (95% CI 7.8–13.2). Based on body mass index (BMI), obesity was more prevalent in females (15.6%; 95% CI 10.7–22.3) than in males (13.3%; 95% CI 8.5–19.5). On the other hand, classifying obesity based on percentage body fat (%BF), 10.6% (95% CI 6.4–16.2) of males and 40.2% (95% CI 34.9–45.3) of females were obese. High waist–hip ratio (WHR) was observed in 9.4% (95% CI 5.4–14.8) of males and 51.1% (95% CI 45.8–56.3) of the females. All individual skinfolds and sum of skinfolds were significantly higher in females (P<0.001). In both males and females above 30 y of age, there was a steep increase in the prevalence of high WHR, and in females, %BF was very high (particularly in %BF quartile>30%). Furthermore, total cholesterol and low-density lipoprotein cholesterol were high in both males and females. Stepwise multiple linear regression analysis showed that for both males and females BMI, WHR and %BF were positive predictors of biochemical parameters, except for HDL-c, for which these parameters were negatively associated.
CONCLUSIONS: Appreciable prevalence of obesity, dyslipidaemia, diabetes mellitus, substantial increase in body fat, generalised and regional obesity in middle age, particularly in females, need immediate attention in terms of prevention and health education in such economically deprived populations.
Similar content being viewed by others
Introduction
Type 2 diabetes, obesity and hyperlipidaemia have been traditionally considered as diseases of affluence. A wealth of data indicates that Asian Indian people abdominal obesity and insulin resistance, and develop glucose intolerance more often.1 The prevalence of diabetes is higher in migrant Asian Indian people as compared to other ethnic groups.2 Some of the studies done on native Indian people also show high prevalence of diabetes in urban areas.3,4 Contribution of dietary practices and lifestyle factors are crucial, making incidence and prevalence of obesity and diabetes mellitus significantly more in the urban population. Recently, considerable concern has been caused by the increasing prevalence of diabetes in India,5 particularly in the urban population.6
High prevalence of malnutrition in people belonging to low socio-economic strata in developing countries led to the assumption that obesity and diabetes will not be a crucial problem in them. Whereas a rural population usually has low risk of development of diabetes and obesity in India,7 their migration to metropolitan cities exposes them to several adverse lifestyle and environmental influences. In cities they usually settle down in urban slums, and take to daily wage jobs. Several lifestyle alterations result from this transition: changes from their traditional penurious eating habits; exposure to severe stress; decreased physical activity; and increase in smoking, tobacco chewing and alcohol intake. Unfortunately, this population has not been researched in detail. A few studies from the developed countries indicate that the prevalence of established risk factors including obesity and diabetes mellitus are higher among men and women with low level of education as a measure of socio-economic status.8 A recent study from the UK records that type 2 diabetes is inversely related to socio-economic strata.9 In this study, the prevalence of diabetes in the least deprived quintile was 13.4 per thousand persons (95% CI 11.44–15.36), compared to 17.22 (95% CI 13.84–17.11) in the most deprived.
However, in developing countries, poverty and scarcity of food is greater, awareness of diseases non-existent, and it appears that these diseases may be equally prevalent in poor people.10,11,12 In one of the largest studies to date, Sawaya et al report obesity in 6.4% of the boys and 8.7% of the girls, in 2411 subjects from 535 families living in the shanty towns of São Paulo, Brazil.13 In this population, there was 30% prevalence of malnutrition, and 78–90% prevalence of stunted growth in children. Even in this population, high prevalence of overweight (16.7%) and obesity (14.1%) was noted in adults.13 Moreover, in 9% of the families, malnutrition in children and obesity in adults co-existed.
To study the lifestyle, anthropometric and metabolic attributes of such a population of low socio-economic strata, we attempted a cross-sectional prevalence survey of obesity, diabetes mellitus, hyperlipidaemia and related lifestyle factors in an urban slum in New Delhi (Delhi Urban Slum Survey), the largest metropolitan city in northern India.
Material and methods
The urban slum colony of Gautam Nagar situated in South Delhi was selected for the study. An approximately 16 square kilometre area includes 4000 dwellings. The total population of the area is approximately 30 000 people. The area was arbitrarily divided into four equal sectors using an electoral list available from the Slum Development Wing, Government of India. The list provided the name, age and address of those eligible for voting (>18 y). Pregnant females, disabled subjects, drug abusers and acutely ill subjects were excluded from the study. The fieldwork was completed within a period of 20 months, starting in January 1998. The first 2 months were taken for training the physicians for various field techniques (eg blood pressure measurement and anthropometric measures), selection of the volunteers and reconnaissance of the slum area. Several visits were made initially to establish contact with the Pradhan (chief of the community) and other prominent people of the community. To establish rapport with the community several medical camps were held in the area, offering free check-ups and medical advice. A pilot survey of knowledge, attitude and practice (KAP survey) carried out at this time revealed that 80–90% of the subjects were unaware of the diseases, their con-sequences and healthy dietary and lifestyle practices.
Two medical teams each consisting of one physician, two technicians and three to four male and female volunteers (recruited from the slum area under study) were assigned two sectors each. The teams visited the every third dwelling, and informed and motivated the eligible household members for the field exercise. Subjects agreeing to participate in the study were instructed to come to a defined clinical area between 7:00 and 9:30 am after 12 h of overnight fasting. In particular, the relevance of the overnight fast was explained to them. Of those approached, only 40% responded. Furthermore, the response of females was better than males in the area, since males go to work quite early in the morning, while females remain behind to do household chores and part-time jobs. All the subjects were fully informed about the purpose of the study. Those detected as having any disease were provided with complete medical investigation and management in the referral hospital free of cost.
A detailed questionnaire incorporating demographic profile, socio-economic data, migration pattern, relevant symptoms, tobacco and alcohol consumption, physical activity pattern, and food frequency questionnaire was administered to the recruited subjects. A complete physical examination was performed on all the subjects. Blood pressure was recorded in sitting position after 5 min rest with a mercury sphygmomanometer according to the standard guidelines. If one abnormal reading was observed, a second reading was recorded after 10 min of rest.
Anthropometric measurements
Weight was measured to the nearest 0.1 kg and height to the nearest 0.1 cm. The body mass index (BMI) was calculated as weight (kg)/height2 (m). Waist circumference was measured midway between iliac crest and lowermost margin of the ribs, and the hip girth was measured at the maximum circumference of buttocks with the subject wearing minimum clothes. The mean of three readings of each was taken for the calculation of waist–hip ratio (WHR). Biceps, triceps, subscapular and suprailiac skinfolds were measured using Lange skinfold callipers. For biceps skinfold, with right arm pendant, the fat pad was measured at the level of the nipple line, and triceps fat pad was measured midway between acromion process of scapula and olecranon process. Fat pads at the inferior angle of scapula, and superiorly on iliac crest directly in the mid-axillary line were measured for sub-scapular and supra-iliac skinfolds. All skinfolds were measured to the nearest 1 mm. A mean of three readings was recorded at each site. Sum of all skinfolds (Σ4SF) and ratios of subscapular and triceps skinfold (SS/TR ratio) and central (sum of subscapular skinfold and suprailiac skinfold) and peripheral (sum of biceps skinfold and triceps skinfold) skinfolds were calculated. Percentage body fat (%BF) was calculated using the standard equation of Durnin and Womersely.14 The equation has been validated for the measurement of %BF in Asian Indians.15
Biochemical samples and analysis
A fasting venous blood sample was obtained after anthropometry and physical examination for blood glucose and lipid profile. Estimation of total cholesterol (TC), serum triglycerides (TG), and high-density lipoprotein cholesterol (HDL-c), was performed on the sample drawn after 12 h overnight fast. TC was estimated with the ferric chloride method.16 The method described by Rosenberg and Gottfried17 was used for the determination of TG. After precipitation of very low-density lipoprotein cholesterol and low-density lipoprotein cholesterol (LDL-c) from the serum by phosphotungstic acid and magnesium chloride, the supernatant was taken and HDL-c estimation performed by the method described for TC. The value of LDL-c was calculated using Friedwald's equation.
Definitions
Obesity was defined as BMI >25 kg/m2.18 %BF was defined as indicative of obesity if it was >25% in males and>30% in females.19,20 WHR of >0.95 for males and >0.80 for females was considered to indicate abdominal obesity.21 High Σ4SF was arbitrarily defined as >50 mm.22 Persistent elevation of blood pressure >140/90 mmHg was defined as hypertension. Dyslipidemias were defined by the criteria laid down by National Cholesterol Education Program, Adult Treatment Panel II.23 Type 2 diabetes mellitus and impaired fasting glucose were diagnosed according to the diagnostic criteria of the American Diabetic Association.24
Statistical methods
Data were entered into an Excel spreadsheet. All the entries were double-checked for any possible keyboard error. For both anthropometric and biochemical parameters, the distribution was confirmed for approximate normality. Mean and standard deviation then summarised the variables. The Z-test was applied to compare the difference in various anthropometric parameters amongst males and females. Correlation between various anthropometric and biochemical parameters was evaluated using Pearson's correlation coefficient. For comparing the mean difference in various anthropometric parameters across three groups as stratified by various biochemical parameters, one-way analysis of variance (ANOVA), followed by a multiple range test was used. Stepwise multiple linear regression analysis was used to determine the anthropometric predictors for biochemical parameters. STATA 6.0, intercooled version (STATA Corporation, Houston, Texas, USA) was used for the statistical analysis. P-value<0.05 was considered as statistically significant.
Observations
Out of 650 subjects screened, 532 subjects (170 males, 362 females) had complete records of clinical profile. Biochemical tests, although performed in all individuals, remained incomplete in a few subjects. Overall, there was a preponderance of Hindu population (91%), followed by Muslims (7%) and Christians (2%). Most of them had migrated from the nearby states, Uttar Pradesh (60%), neighbouring townships of Delhi (13%), Rajasthan (6%) and others. The reason for migration was the search for better economic prospects.
The demographic profile of the study population is shown in Table 1. Approximately sixteen percent of the males were unemployed and the majority of the rest belonged to the labourer class (Table 1). The majority of the females were housewives followed by household workers (Table 1). Seventeen percent of the males and 63.5% of the females were not earning. The monthly income of majority of males was below 3000 rupees (∼US$70), and in females it was below 2000 rupees (∼US$45; Table 1). Prominently, approximately 70% of the males were smokers or chewed tobacco regularly. Most people were staying in one or two room temporary hutments, with extremely poor sanitary and hygienic conditions. There were no proper medical facilities in the area; however, there were a few practitioners of alternative medicine (Ayurveda and homeopathy). People with medical problems approached these practitioners first, as they dispense medicines at cheap rates.
Impaired fasting glucose (IFG) was observed more in females as compared to males, although the difference was not statistically significant (Table 1). Type 2 diabetes was observed in 11.2% (95% CI 6.8–16.9) and 9.9% (95% CI 7.0–13.5) of males and females, respectively; the overall prevalence being 10.3% (95% CI 7.8–13.2). Prevalence of hypertension was similar in both males and females (Table 1). Hypercholesterolaemia was observed in a high number of males (26.8%; 95% CI 20.2–34.3) and females (27.5%; 95% CI 22.9–32.5), and similarly equally high number of subjects had high LDL-c levels (Table 1). However, hypertriglyceridaemia was observed more often in males, although the difference was statistically not significant. Further, 15.8% (95% CI 10.5–22.4) males and 16.7% (95% CI 12.8–21.1) female subjects showed low levels of HDL-c (Table 1).
The anthropometric and body fat profile of the study population has been shown in Tables 2 and 3. By the measurement of BMI alone, obesity was more prevalent in females (15.6%; 95% CI 12.0–19.8) than males (13.3%; 95% CI 8.5–19.5; Table 3). The overall prevalence of obesity was 13.9% (95% CI 11.1–17.2). Taking %BF as the measurement of obesity, 10.6% (95% CI 6.4–16.3) males and 40.2% (95% CI 35.0–45.4) females were classified as obese. The overall prevalence of obesity, determined by %BF, was 30.7% (95% CI 26.8–34.8; Table 3). The mean BMI of males and females were comparable. WHR was higher in females, although the difference was statistically insignificant. High WHR was observed in 51.1% (95% CI 45.8–56.3) of the females and 9.4% (95% CI 5.5–14.8) of the males (Table 3). There was a significant difference in the values of the biceps, triceps, subscapular and supra-iliac skinfolds, all values being higher in females. Σ4SF was also higher in females as compared to males (P<0.001). Moreover, high Σ4SF was observed in 30.8% (95% CI 23.9–38.3) of males as compared to 54.6% (95% CI 49.2–59.7) of females. SS-TR was higher in males as compared to females (P<0.001; Table 2).
Prevalence of diabetes increased with advancing age (Table 3). The subjects were stratified according to the age groups: 18–30 y, 31–50 y and 51 y and above. BMI and %BF were further categorised into four approximate quartiles (BMI—<18, 18–23, 23.1–24.9 and ≥25 kg/m2, %BF—<18, 18–25, 25.1–30 and >30%; Table 3). In females, there was a significantly increasing trend in the prevalence of obesity as defined by BMI, with advancing age (chi-square for trends=4.5, P<0.05); the highest being in the 51 y and above age group (22.2%). In males, the prevalence of obesity was highest in the age group of 31–50 y. There was a steeper rise in the WHR after 30 y of age, particularly in females. Of note, 15.5% males and 60% females had high WHR in the 31–50 y age group, increasing by 18% as compared to females aged 18–30 y. In females aged 51 y and above it increased further to 66.7%. Similar to BMI-defined obesity, %BF-defined obesity also showed a significant increasing trend with advancing age (chi-square for trends=14.1, P<0.001). In females it was noticed to be high even in the younger age group (29.9%), and increased remarkably to approximately 50% in the middle aged and elderly. The magnitude of increase was mostly observed in highest quartile of %BF. In contrast, the percentage of males with high %BF remained stable in the range of 8–11.5% across the age groups (Table 3).
On comparing the various anthropometric measures across the BMI quartiles, a progressive increase in the mean values with increase in BMI in both males and females was observed (Table 4). Of particular interest is the increase in mean value of %BF across the BMI quartiles in both males and females (Table 4). No similar trend of increase in prevalence of glucose intolerance and lipid abnormalities was observed with increase in BMI in either sex. The metabolic abnormalities were observed more often in subjects belonging to the BMI quartile of >18–23 kg/m2; however, numbers of subjects in the upper two quartiles of BMI were smaller (Table 4).
Multivariate regression analysis was applied to determine the anthropometric predictors of biochemical parameters. Age was considered as a confounding variable and it was forced into the stepwise regression model. BMI was observed to be a significant positive predictor of fasting blood glucose for both males and females in this model. Further, it was a significant positive predictor of TC in females. For serum TG, both BMI and %BF were significant positive predictors in females. WHR and %BF were negatively associated with HDL-c in both males and females (Table 5).
Discussion
The remarkably high prevalence of obesity in the study population is of particular note despite their poor socio-economic strata. Although the mean BMIs are in the range of 20–21, the prevalence of obesity, as defined by BMI, is high. Moreover, high WHR is noteworthy, both in males and, particularly, females.
The prevalence of obesity recorded in the current study is lower compared to that recorded (27.8%) in an urban sample of adults in New Delhi.25 Unfortunately, few comparable studies performed in the urban slums are available in the literature. Studies from developed countries indicate higher prevalence of atherosclerosis risk factors among men and women with lower socio-economic status.8 In developing countries, the problem of poverty and scarcity of food is particularly acute in the slum areas. In the Klong Toey slums of Bangkok, 25.5% of the subjects were overweight and 10% were obese.10,11 A study involving women in a low-income area in Karachi showed 42 and 8% of women to be overweight and have abdominal obesity respectively,12 an observation similar to the current study. Sawaya et al reported high prevalence of obesity and malnutrition coexisting in the same population.13
Estimations of individual skinfolds in the current study show comparatively lower values when compared to those recorded in South Asian men and women in the UK, having mean BMI in the range of 25–26,1 indicating more subcutaneous fat in the immigrant Asian Indian people in the UK. Although desirable and much needed, data on skinfolds of rural and urban native Indian population are not available. In the current study, the ratio of central vs peripheral skinfolds is greater in males due to excess truncal fat, and this is also reflected by higher SS/TR ratios. However, WHR was higher in females, indicating excess abdominal fat even in females. Mean WHR is lower in males, and higher in females as compared to Asian Indian people in the UK.1 Of further interest is the remarkable increase in the prevalence of high WHR in middle-aged females, with no appreciable increase in their BMI. In males, WHR increased with increase in age from 30 to 50 y (Table 3). More than a third of the population over 30 y of age having abdominal obesity is of considerable concern because of associated metabolic and cardiovascular consequences.
The detailed observations on anthropometric measurements and %BF have rarely been explored in the studies done on Asian Indian people living in India. The most striking observation in the current study is high %BF in females. In males, only 10.6% had excess %BF, a figure generally approximating the percentage prevalence of high BMI in this group. There is, however, a marked discordance between the two measures of obesity in females; 40.2% show %BF more than 30%, while only 15.6% show BMI higher than 25. The most striking observation is the increase in body fat with advancing age (about 50% had high body fat above the age of 30 y). The conspicuous feature in women, therefore, is under-representation of obesity when defined by BMI alone. These observations are of considerable practical relevance, questioning BMI as a valid epidemiological tool in Asian Indian population, particularly in females. Further, all the metabolic complications of excess fat are likely to be present in these women with high body fat, even when their BMI is in a normal range. Such women, when postmenopausal and without the benefit of hormonal protection, are more likely to develop occlusive consequences of atherosclerosis.
Variable prevalence (3–11.2%) of diabetes has been reported from urban areas of India depending upon on the region, caste and type of survey, diagnostic tool and diagnostic terminology.6,7 In the urban population of Delhi, the prevalence of diabetes mellitus ranged from 1.6 to 9%, being more common in obese subjects.25 In the rural Indian population, it is reported to be in the range of 1–5%.7,26,27 In one of the well-designed studies in rural areas of North Arcot District in south India, the prevalence of impaired glucose tolerance (IGT) and diabetes mellitus was 6.6 and 4.9%, respectively, as investigated by 2 h post-75 g oral glucose load values.27 Similarly, in a rural community in the state of Punjab, only 4.6% were diabetic.28 It is also noteworthy that the prevalence of IFG is greater in females as compared to males in the current study, although it was statistically insignificant. In a recent study from Kashmir valley, authors record higher prevalence of IGT and diabetes mellitus in females as well.29 The observed prevalence of IFG and diabetes mellitus in the present study is higher than that reported from the rural population, and equal to or more than that observed in the urban population. However, it is difficult to compare most studies done in India, since diagnostic criteria of diabetes, methodology of tests, and sampling modes were different. Nonetheless, the prevalence of IFG and type 2 diabetes mellitus in this sample of urban slum population is impressive.
Similarly, in the present study, the high prevalence of dyslipidaemia is striking. Studies from various parts of India again reveal differences in the prevalence. For example, 7.1% of the subjects had hypercholesterolaemia in a rural community in northern state of Punjab.28 Of specific concern are approximately 27% of the subjects with high levels of total cholesterol in the current study. While BMI, and %BF correlated to serum lipid levels more in females, correlation was better observed with %BF in males. Since most of the subjects are not likely to be tested for blood lipids due to either unawareness of the diseases and/or economic constraints, undetected hypercholesterolaemia, coupled with low levels of HDL-c, generalised and abdominal obesity, and hypertension are harbingers of accelerated atherosclerosis.
What is the cause of high prevalence of obesity and other risk factors in this poor population? Certainly, there is a considerable shift in their dietary and lifestyle profile. The dietary profile is changed to a mixture of rural and urban diets, with higher consumption of saturated fat and low intake of fibre. Further, most of these people used to be hard working farmers in the fields in their villages, and have changed to sitting around on the roadside as vendors, thus radically changing their activity profile. Barker's hypothesis may also be invoked to explain these observations.30,31 Although originally reported from the developed countries, these observations have now been recorded from the Indian subcontinent as well.32,33 The metabolic effects of adverse in-utero environment and low birth weight appear in childhood and adolescence, and may be further exacerbated in the face of deteriorating lifestyle factors. Such a situation is likely to occur in economically deprived people who move from the villages to large cities. Further, activation of hypothalamus–pituitary–adrenocortical axis is known to occur due to adverse socio-economic circumstances, which is often combined with psychosocial stress and ‘physiological defeat reaction’.34,35 Increased WHR and generalised obesity may thus result.36
Economic deprivation and poor living conditions in villages lure people to the cities, and such migration has been increasing rapidly in India. As estimated in 1995, 30–50% of the population of many cities in India reside in the urban slums. Approximately 23 such cities have populations exceeding the million mark, and the current estimate of their total population would be close to 100 million.37 One can thus judge the burden of the slum population, and magnitude of their health problems. Chronic afflictions such as diabetes and coronary heart disease (CHD) are difficult diseases to handle by poor people on a long-term basis. Availability of cheap but standard care (eg government hospitals) is often difficult to access because of long travel distance, patient crowding, understaffing and non-availability of drugs and equipment. As a result they often seek the help of ‘quacks’ and other unqualified practitioners of medicine. Further, absence from work deprives them of their wages, and treatment of the diseases and its complications poses extreme hardship from which the individual and his/her family never recovers.
The non-communicable diseases, particularly the upsurge of diabetes mellitus, hypertension and CHD pose a grim challenge to India in this century. Findings of the present study are particularly ominous, and dispel the notion that the policy makers need to be concerned only about communicable diseases in the people of low socio-economic strata in urban slums. There is, therefore, an urgent need for concerted governmental and non-governmental efforts and firm political will to tackle this important problem. Moreover, further studies are needed to delineate the problem in detail and specify the adverse factors, particularly the changes in the nutrition and activity profile.
References
McKeigue PM, Shah B, Marmot MG . Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians Lancet 1991 337: 382–388.
Ramaiya K, Kodali VRR, Alberti, KGMM . Epidemiology of diabetes in Asians of the Indian Subcontinent Diabetes Metab Rev 1990 6: 125–146.
Ramachandran A, Jali MV, Mohan V, Snehalatha C . High prevalence of diabetes in an urban population in South India Br Med J 1986 297: 587–590.
Varma NPS, Mehta SP, Madhu SV, Mather HM, Keen H . Prevalence of known diabetes in an urban Indian environment: the Darya Ganj diabetes survey Br Med J 1986 293: 423–424.
King H, Aubert RE, Herman WH . Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections Diabetes Care 1998 21: 1414–1431.
Ramachandran A, Snehalatha C, Latha E, Vijay V, Viswanathan M . Rising prevalence of NIDDM in an urban population in India Diabetologia 1997 40: 232–237.
Gupta OP, Joshi MH, Dave SK . Prevalence of diabetes in India Adv Metab Disord 1978 9: 147–165.
Millar WJ, Wigle DT . Socio-economic disparities in risk factors for cardiovascular diseases CMAJ 1986 134: 127–132.
Connolly V, Unwin N, Sherriff P, Bilous R, Kelly W . Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type II diabetes in the deprived areas J Epidemiol Community Health 2000 54: 173–177.
Bunnag SC, Amorn SC, Chandraprasert S . The prevalence of obesity, risk factors and associated disease in Klong Toey slum and Klong Toey government apartment houses Diabetes Res Clin Pract 1990 10: (Suppl 1): S81–87.
Sitthi-Amorn C, Chandraprasert S, Bunnag SC, Plengvidhya SC . The prevalence and risk factors of hypertension in Klon Toey slum and Klong Toey government apartment houses Int J Epidemiol 1989 18: 89–94.
Akatsu H, Aslam A . Prevalence of hypertension and obesity among women over age 25 in a low income area in Karachi, Pakistan J Pak Med Assoc 1996 46: 191–193.
Sawaya AL, Dallal G, Solymos G et al. Obesity and malnutrition in a shantytown population in the city of Sao Paulo, Brazil Obes Res 1995 3: (suppl 2): 135s–143s.
Durnin JVGA, Womersely J . Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 y Br J Nutr 1974 32: 77–97.
Kuriyan R, Petracchi C, Ferro-Luzzi A, Shetty PS, Kurpad AV . Validation of expedient methods for measuring body composition in Indian adults Ind J Med Res 1998 107: 37–45.
Chiamori N, Henry RJ . Study of the ferric chloride method for determination of total cholesterol and cholesterol esters Am J Clin Pathol 1959 31: 305–309.
Rosenberg SP, Gottfried A . Improved manual spectrophotometric procedure for determination of triglycerides Clin Chem 1973 9: 1077–1078.
World Health Organization . The Asia-Pacific perspective. Redefining obesity and its treatment International Diabetes Institute. February 2000
Hortobagyi T, Israel RG, O'Brien KF . Sensitivity and specificity of the Quetelet index to assess obesity in men and women Eur J Clin Nutr 1994 48: 769–775.
Pollock ML, Wilmore JH . Exercise in health and disease WB Saunders: Philadelphia, PA 1990
Willett WC, Dietz WH, Colditz GA . Guidelines for healthy weight New Engl J Med 1999 341: 427–434.
Dudeja V, Misra A, Pandey RM, Devina G, Kumar G, Vikram NK . Body mass index does not accurately predict overweight in Asian Indians in Northern India Br J Nutr (in press).
National Cholesterol Education Panel . Second report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Pressure in Adults (Adult Treatment Panel II) Circulation 1994 89: 1329–1445.
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: report of the Expert Committee on Diagnosis and Classification of Diabetes Mellitus . Diabetes Care 1997 20: 1183–1197.
Gopinath N, Chadha SL, Jain P, Shekhawat S, Tandon R . An epidemiological study of obesity in adults in the urban population of Delhi J Assoc Phys Ind 1994 42: 212–215.
Tripathy BB, Panda NC, Tej SC, Sahoo GN, Kar BN . Survey for the detection of glycocusira, hyperglycemia, and diabetes mellitus in urban and rural areas of Cuttak district J Assoc Phys Ind 1971 19: 681–692.
Patandin S, Bots ML, Abel R, Valkenburg HA . Impaired glucose intolerance and diabetes mellitus in a rural population in South India Diabetes Res Clin Pract 1994 24: 47–53.
Wander GS, Khurana SB, Gulati R, Sachar RK, Gupta RK, Khurana S, Anand IS . Epidemiology of coronary heart disease in a rural Punjab population-prevalence and correlation with various risk factors Indian Heart J 1994 46: 319–323.
Zargar AH, Khan AK, Masoodi SR, Laway BA, Wani AI, Bashir MI, Dar FA . Prevalence of type 2 diabetes mellitus and impaired glucose tolerance in the Kashmir Valley of the Indian subcontinent Diabetes Res Clin Pract 2000 47: 135–146.
Hales CN, Barker DJ, Clark PM, Cox LJ, Fall C, Osmond C, Winter PD . Fetal and infant growth and impaired glucose tolerance at age 64 Br Med J 1991 303: 1019–1022.
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM . Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidemia (syndrome X): relation to reduced fetal growth Diabetologia 1993 36: 62–67.
Fall CH, Stein CE, Kumaran K, Cox V, Osmond C, Barker DJ, Hales CN . Size at birth, maternal weight, and type 2 diabetes in South India Diabetic Med 1998 15: 220–227.
Yajnik CS, Fall CH, Vaidya U, Pandit AN, Bavdekar A, Bhat DS, Osmond C, Hales CN, Barker DJ . Fetal growth and glucose and insulin metabolism in four-year-old Indian children Diabetic Med 1995 12: 330–336.
Bjorntorp P . Behavior and metabolic disease Int J Behav Med 1996 3: 285–302.
Bjorntorp P . Visceral fat accumulation: the missing link between psychosocial factors and cardiovascular disease? J Intern Med 1991 230: 195–201.
Brunner EJ, Marmot MG, Nanchahal K, Shipley MJ, Stansfeld SA, Juneja M, Alberti KG . Social inequality in coronary risk: central obesity and the metabolic syndrome: evidence from the Whitehall II study Diabetologia 1997 40: 1341–1349.
Tribhuvan RD, Kelkar A . Health issues of slum women. In: Tribhuvan RD (ed.). Social problems and development issues in slum women Amruta: Pune 1997 pp 66–75.
Acknowledgements
The study was fully supported by financial grant from Science and Society Division, Department of Science and Technology, Ministry of Science and Technology, Government of India. The authors express their appreciation to the staff of SRB Centre of Clinical Pharmacology, Department of Medicine, All India Institute of Medical Sciences, New Delhi including Mr Ramesh Giri, Mr Inder Taneja, Mr Gian Chand and Mrs Alice Jacob for performing various investigations, Mr RL Taneja for performing quality control of various biochemical tests, Mrs Jyoti for typing and Miss Kajal for editing the manuscript. Help and voluntary services provided from the volunteers, in particular the late Mr Jaipal, and the population of the slum community is appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Misra, A., Pandey, R., Rama Devi, J. et al. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes 25, 1722–1729 (2001). https://doi.org/10.1038/sj.ijo.0801748
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801748
Keywords
This article is cited by
-
Prevalence and risk factors for dyslipidemia among South Indian adults: A community based-NCD study
International Journal of Diabetes in Developing Countries (2023)
-
Tobacco chewing and associated factors among a vulnerable youth population in Sri Lanka
BMC Public Health (2022)
-
Unequal burden of equal risk factors of diabetes between different gender in India: a cross-sectional analysis
Scientific Reports (2021)
-
Comparison of clinical features, complication profile, and achievement of guideline targets in early- and late-onset type 2 diabetes patients from North India
International Journal of Diabetes in Developing Countries (2021)
-
Health issues in a Bangalore slum: findings from a household survey using a mobile screening toolkit in Devarajeevanahalli
BMC Public Health (2019)