Abstract
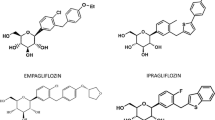
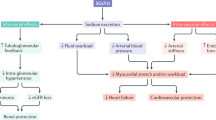
Inhibitors of sodium-glucose cotransporters type 2 (SGLT2) are proposed as a novel approach for the management of type 2 diabetes mellitus. SGLT2 cotransporters are responsible for reabsorption of 90 % of the glucose filtered by the kidney. The glucuretic effect resulting from SGLT2 inhibition contributes to reduce hyperglycaemia and also assists weight loss and blood pressure reduction. Several SGLT2 inhibitors are already available in many countries (dapagliflozin, canagliflozin, empagliflozin) and in Japan (ipragliflozin, tofogliflozin). These SGLT2 inhibitors share similar pharmacokinetic characteristics with a rapid oral absorption, a long elimination half-life allowing once-daily administration, an extensive hepatic metabolism mainly via glucuronidation to inactive metabolites and a low renal elimination as a parent drug. Pharmacokinetic parameters are slightly altered in the case of chronic kidney disease (CKD). While no dose adjustment is required in the case of mild CKD, SGLT2 inhibitors may not be used or only at a lower daily dose in patients with moderate CKD. Furthermore, the pharmacodynamic response to SGLT2 inhibitors as assessed by urinary glucose excretion declines with increasing severity of renal impairment as assessed by a reduction in the estimated glomerular filtration rate. Nevertheless, the glucose-lowering efficacy and safety of SGLT2 inhibitors are almost comparable in patients with mild CKD as in patients with normal kidney function. In patients with moderate CKD, the efficacy tends to be dampened and safety concerns may occur. In patients with severe CKD, the use of SGLT2 inhibitors is contraindicated. Thus, prescribing information should be consulted regarding dosage adjustments or restrictions in the case of renal dysfunction for each SGLT2 inhibitor. The clinical impact of SGLT2 inhibitors on renal function and their potential to influence the course of diabetic nephropathy deserve attention because of preliminary favourable results in animal models.
Similar content being viewed by others
References
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–9.
Tahrani AA, Bailey CJ, Del Prato S, et al. Management of type 2 diabetes: new and future developments in treatment. Lancet. 2011;378(9786):182–97.
Bonnet F, Scheen AJ. SGLT-2 inhibitors: an opportunity to renew our therapeutic strategy for type 2 diabetes ? Diabetes Metab. 2014;40(Suppl):S1–3.
Neumiller JJ, White JR Jr, Campbell RK. Sodium-glucose co-transport inhibitors: progress and therapeutic potential in type 2 diabetes mellitus. Drugs. 2010;70(4):377–85.
Tahrani AA, Barnett AH, Bailey CJ. SGLT inhibitors in management of diabetes. Lancet Diabetes Endocrinol. 2013;1(2):140–51.
Hasan FM, Alsahli M, Gerich JE. SGLT2 inhibitors in the treatment of type 2 diabetes. Diabetes Res Clin Pract. 2014;104(3):297–322.
Bailey CJ. Renal glucose reabsorption inhibitors to treat diabetes. Trends Pharmacol Sci. 2011;32(2):63–71.
Abdul-Ghani MA, Norton L, Defronzo RA. Role of sodium-glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetes. Endocr Rev. 2011;32(4):515–31.
Scheen AJ, Paquot N. Metabolic effects SGLT2 inhibitors beyond increased glucosuria: a review of clinical evidence. Diabetes Metab. 2014;40(Suppl):S4–11.
Vasilakou D, Karagiannis T, Athanasiadou E, et al. Sodium-glucose cotransporter 2 inhibitors for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med. 2013;159(4):262–74.
Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
Nauck MA. Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Des Devel Ther. 2014;8:1335–80.
Scheen AJ. Pharmacodynamics, efficacy and safety of SGLT2 inhibitors for the treatment of type 2 diabetes. Drugs. 2015;75(1):33–59.
Scheen AJ. Evaluating SGLT2 inhibitors for type 2 diabetes: pharmacokinetic and toxicological considerations. Expert Opin Drug Metab Toxicol. 2014;10(5):647–63.
Scheen AJ. Drug-drug interactions with SGLT-2 inhibitors, new oral glucose-lowering agents for the management of type 2 diabetes. Clin Pharmacokinet. 2014;53(4):295–304.
Plosker GL. Dapagliflozin: a review of its use in type 2 diabetes mellitus. Drugs. 2012;72(17):2289–312.
Kasichayanula S, Liu X, Lacreta F, et al. Clinical pharmacokinetics and pharmacodynamics of dapagliflozin, a selective inhibitor of sodium-glucose co-transporter type 2. Clin Pharmacokinet. 2014;53(1):17–27.
Plosker GL. Dapagliflozin: a review of its use in patients with type 2 diabetes. Drugs. 2014;74(18):2191–209.
Elkinson S, Scott LJ. Canagliflozin: first global approval. Drugs. 2013;73(9):979–88.
Lamos EM, Younk LM, Davis SN. Canagliflozin, an inhibitor of sodium-glucose cotransporter 2, for the treatment of type 2 diabetes mellitus. Expert Opin Drug Metab Toxicol. 2013;9(6):763–75.
Plosker GL. Canagliflozin: a review of its use in patients with type 2 diabetes mellitus. Drugs. 2014;74(7):807–24.
Scheen AJ. Pharmacokinetic and pharmacodynamic profile of empagliflozin, a sodium glucose co-transporter 2 inhibitor. Clin Pharmacokinet. 2014;53(3):213–25.
Seman L, Macha S, Nehmiz G, et al. Empagliflozin (BI 10773), a potent and selective SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Drug Devel. 2013;2(2):152–61.
Scott LJ. Empagliflozin: a review of its use in patients with type 2 diabetes mellitus. Drugs 2014 (Epub 2014/10/03).
Poole RM, Dungo RT. Ipragliflozin: first global approval. Drugs. 2014;74(5):611–7.
Markham A, Elkinson S. Luseogliflozin: first global approval. Drugs. 2014;74(8):945–50.
Poole RM, Prossler JE. Tofogliflozin: first global approval. Drugs. 2014;74(8):939–44.
Scheen AJ. Pharmacokinetic considerations for the treatment of diabetes in patients with chronic kidney disease. Expert Opin Drug Metab Toxicol. 2013;9(5):529–50.
Kohan DE, Fioretto P, Tang W, et al. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int. 2014;85(4):962–71.
Maliha G, Townsend RR. SGLT2 inhibitors: their potential reduction in blood pressure. J Am Soc Hypertens. 2015;9(1):48–53.
Vallon V, Thomson SC. Renal function in diabetic disease models: the tubular system in the pathophysiology of the diabetic kidney. Annu Rev Physiol. 2012;74:351–75.
De Nicola L, Gabbai FB, Liberti ME, et al. Sodium/glucose cotransporter 2 inhibitors and prevention of diabetic nephropathy: targeting the renal tubule in diabetes. Am J Kidney Dis. 2014;64(1):16–24.
Stanton RC. Sodium glucose transport 2 (SGLT2) inhibition decreases glomerular hyperfiltration: is there a role for SGLT2 inhibitors in diabetic kidney disease? Circulation. 2014;129(5):542–4.
European Medicines Agency. Assessment report. Forxiga (dapagliflozin). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002322/WC500136024.pdf. Accessed 2 Mar 2015.
European Medicines Agency. Assessment report. Canagliflozin. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002649/WC500156456.pdf. Accessed 2 Mar 2015.
European Medicines Agency. Assessment report: Jardiance. International non-proprietary name: empagliflozin. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002677/WC500168592.pdf. Accessed 2 Mar 2015.
Kasichayanula S, Liu X, Pe Benito M, et al. The influence of kidney function on dapagliflozin exposure, metabolism and pharmacodynamics in healthy subjects and in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2013;76(3):432–44.
Ptaszynska A, Mansfield T, Apanovitch AM, et al. Dapagliflozin, selective SGLT2 inhibitor, does not increase risk of fractures. Diabetes. 2014;63(Suppl 1):A282 (abstract 1085-P).
Ptaszynska A, Johnsson KM, Parikh SJ, et al. Safety profile of dapagliflozin for type 2 diabetes: pooled analysis of clinical studies for overall safety and rare events. Drug Saf. 2014;37(10):815–29.
Ptaszynska A, Mansfield T, Johnsson E, et al. Long-term renal safety with dapagliflozin treatment. Diabetologia. 2014;57(Suppl 1):S22 (abstract 798).
Johnsson E, Johnsson KM, Mansfield TA, et al. Diuresis-related safety and tolerability of dapagliflozin in type 2 diabetes mellitus over 24 weeks. Diabetologia. 2014;57(Suppl 1):S323 (abstract 800).
Yavin Y, Mansfield TA, Ptaszynska A, et al. Hyperkalemia incidence with the SGLT2 inhibitor dapagliflozin. Diabetes. 2014;63(Suppl 1):A282 (abstract 1086-P).
Lambers Heerspink HJ, de Zeeuw D, Wie L, et al. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab. 2013;15(9):853–62.
Oliva RV, Bakris GL. Blood pressure effects of sodium-glucose co-transport 2 (SGLT2) inhibitors. J Am Soc Hypertens. 2014;8(5):330–9.
Thomas MC. Renal effects of dapagliflozin in patients with type 2 diabetes. Ther Adv Endocrinol Metab. 2014;5(3):53–61.
Devineni D, Curtin CR, Marbury TC, et al. Effect of hepatic or renal impairment on the pharmacokinetics of canagliflozin, a sodium glucose co-transporter 2 inhibitor. Clin Ther. 2015. doi:10.1016/j.clinthera.2014.12.013 (Epub ahead of print).
Inagaki N, Kondo K, Yoshinari T, et al. Pharmacokinetic and pharmacodynamic profiles of canagliflozin in Japanese patients with type 2 diabetes mellitus and moderate renal impairment. Clin Drug Investig. 2014;34(10):731–42.
Devineni D, Vaccaro N, Polidori D, et al. Effects of hydrochlorothiazide on the pharmacokinetics, pharmacodynamics, and tolerability of canagliflozin, a sodium glucose co-transporter 2 inhibitor, in healthy participants. Clin Ther. 2014;36(5):698–710.
Roussel R, de Zeeuw D, Law G, et al. Efficacy and safety of canagliflozin (CANA) in patients with type 2 diabetes mellitus (T2DM) who progressed to stage 3A chronic kidney disease during treatment (abstract). Diabetologia. 2014;57(Suppl 1):S322–3 (abstract 799).
Yale JF, Bakris G, Cariou B, et al. Efficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes Metab. 2013;15(5):463–73.
Yale JF, Bakris G, Cariou B, et al. Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes mellitus and chronic kidney disease. Diabetes Obes Metab. 2014;16(10):1016–27.
Yamout H, Perkovic V, Davies M, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes and stage 3 nephropathy. Am J Nephrol. 2014;40(1):64–74.
Khurana M, Vaidyanathan J, Marathe A, et al. Canagliflozin use in patients with renal impairment: utility of quantitative clinical pharmacology analyses in dose optimization. J Clin Pharmacol. 2015. doi:10.1002/jcph.466. (Epub ahead of print).
Macha S, Mattheus M, Halabi A, et al. Pharmacokinetics, pharmacodynamics and safety of empagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, in subjects with renal impairment. Diabetes Obes Metab. 2014;16(3):215–22.
Sarashina A, Ueki K, Sasaki T, et al. Effect of renal impairment on the pharmacokinetics, pharmacodynamics, and safety of empagliflozin, a sodium glucose cotransporter 2 inhibitor, in Japanese patients with type 2 diabetes mellitus. Clin Ther. 2014;36(11):1606–15.
Barnett AH, Mithal A, Manassie J, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2(5):369–84.
Tikkanen I, Narko K, Zeller C, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38(3):420–8.
Cherney D, von Eynatten M, Lund SS, et al. Sodium glucose transporter 2 inhibition with empagliflozin reduces microalbuminuria in patients with type 2 diabetes (abstract). Diabetologia. 2014;57(Suppl 1):S333 (abstract 823).
Cherney DZ, Perkins BA, Soleymanlou N, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
Ridderstrale M, Svaerd R, Zeller C, et al. Rationale, design and baseline characteristics of a 4-year (208-week) phase III trial of empagliflozin, an SGLT2 inhibitor, versus glimepiride as add-on to metformin in patients with type 2 diabetes mellitus with insufficient glycemic control. Cardiovasc Diabetol. 2013;12(1):129.
Kadokura T, Zhang W, Krauwinkel W, et al. Clinical pharmacokinetics and pharmacodynamics of the novel SGLT2 inhibitor ipragliflozin. Clin Pharmacokinet. 2014;53(11):975–88.
Ferrannini E, Veltkamp SA, Smulders RA, et al. Renal glucose handling: impact of chronic kidney disease and sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care. 2013;36(5):1260–5.
Kashiwagi A, Takahashi H, Ishikawa H, et al. A randomized, double-blind, placebo-controlled study on long-term efficacy and safety of ipragliflozin treatment in patients with type 2 diabetes mellitus and renal impairment: results of the Long-Term ASP1941 Safety Evaluation in Patients with Type 2 Diabetes with Renal Impairment (LANTERN) study. Diabetes Obes Metab. 2015;17(2):152–60.
Zell M, Husser C, Kuhlmann O, et al. Metabolism and mass balance of SGLT2 inhibitor tofogliflozin following oral administration to humans. Xenobiotica. 2014;44(4):369–78.
Schwab D, Portron A, Backholer Z, et al. A novel double-tracer technique to characterize absorption, distribution, metabolism and excretion (ADME) of [14C]tofogliflozin after oral administration and concomitant intravenous microdose administration of [13C]tofogliflozin in humans. Clin Pharmacokinet. 2013;52(6):463–73.
Schwab D, Portron A, Fukushima Y, et al. Tofogliflozin a selective SGLT2 inhibitor exhibits highly favourable drug properties for use in patients with renal impairment and for combination with other medicines. Diabetologia. 2012;55(Suppl 1):S316 (abstract 767).
Sasaki T, Seino Y, Fukatsu A, et al. Safety, pharmacokinetics, and pharmacodynamics of single and multiple luseogliflozin dosing in healthy Japanese males: a randomized, single-blind, placebo-controlled trial. Adv Ther. 2014;31(3):345–61.
Haneda M, Seino Y, Inagaki N, et al. Efficacy and safety of luseogliflozin in various levels of renal function in Japanese patients with type 2 diabetes mellitus: analysis of pooled data from long-term phase 3 trials. Diabetes. 2014;63(Suppl 1):A267 (abstract 1035-P).
Miao Z, Nucci G, Amin N, et al. Pharmacokinetics, metabolism, and excretion of the antidiabetic agent ertugliflozin (PF-04971729) in healthy male subjects. Drug Metab Dispos. 2013;41(2):445–56.
Kapur A, O’Connor-Semmes R, Hussey EK, et al. First human dose-escalation study with remogliflozin etabonate, a selective inhibitor of the sodium-glucose transporter 2 (SGLT2), in healthy subjects and in subjects with type 2 diabetes mellitus. BMC Pharmacol Toxicol. 2013;14:26.
Funding and conflict of interest
No sources of funding were used to assist in the preparation of this manuscript. No conflicts of interest are directly relevant to the content of this manuscript.
A. J. Scheen has received lecture/advisor fees from AstraZeneca/BMS, Boehringer Ingelheim, Eli Lilly, Janssen, Merck Sharp & Dohme, Novartis, NovoNordisk, Sanofi-Aventis and Takeda.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scheen, A.J. Pharmacokinetics, Pharmacodynamics and Clinical Use of SGLT2 Inhibitors in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease. Clin Pharmacokinet 54, 691–708 (2015). https://doi.org/10.1007/s40262-015-0264-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-015-0264-4