Background
Surgery in patients with super-obesity (BMI ≥50) involves technical difficulties that are related, among other factors, to increased liver volume. Although the intragastric balloon is not a definitive alternative to surgery, it has been used in these patients as a primary therapeutic means of reducing excess weight and the risks of subsequent surgery. It has also been reported to considerably diminish liver volume to facilitate technical aspects of the operation. We evaluated preoperative weight loss in patients with super-obesity after placement of an intragastric balloon and its effect on liver volume measured by computed axial tomography (CT) prior to laparoscopic Roux–en–Y gastric bypass (LRYGBP).
Methods
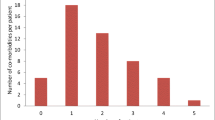
The balloon was implanted preoperatively under endoscopic guidance and sedation in 31 patients with super-obesity, to reduce weight prior to LRYGBP. Two patients were excluded from the study for intolerance and the balloon was removed 2 weeks after placement. Measurement of liver volume was done with axial images obtained by spiral CT with a section thickness of 10 mm, reconstitution index 10 mm, pitch 1.5 and acquisition delay 60 seconds.Volumes were calculated using the sum of areas technique. Measurement of volume was done in these 29 patients prior to balloon placement and the week before surgery.
Results
After placement of the balloon, 27 patients (93%) had nausea and 25 patients (86%) had vomiting, which abated 1 week after placement. Mean liver volume prior to balloon placement was 2938.53 ± 853.1 cm3, which at 6 weeks dropped to values of 1918.2 ± 499.8 cm3, revealing a considerable reduction in liver volume [31.8% ± 18.16% (range 3.1%–58.5%)]. Percent of excess weight loss was 22.14% ± 7.39. LRYGBP was performed at 6 months.
Conclusions
In patients with super-obesity, preoperative treatment with intragastric balloon considerably reduces liver volume to facilitate LRYGBP.
Similar content being viewed by others
References
Clark JM. The epidemiology of non-alcoholic fatty liver disease in adults. J Clin Gastroenterol 2006; 40 (Suppl 1): S5–S10.
Shaffer EA. Bariatric surgery: a promising solution for non-alcoholic steatohepatitis in the very obese. J Clin Gastroenterol 2006; 40 (Suppl 1): S44–S50.
Alfalah H, Philippe B, Ghazal F et al. Intragastric balloon for preoperative weight reduction in candidates for laparoscopic gastric bypass with massive obesity. Obes Surg 2006; 16:147–50.
Bussetto L, Segato G, De Luca M et al. Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: a case-control study. Obes Surg 2004; 14: 671–6.
Lujan JA, Hernández Q, Frutos MD et al. Laparoscopic gastric bypass in the treatment of morbid obesity. Surg Endosc 2002; 16:1658–62.
Ogunnaike BO, Jones SB, Jones DB et al. Anesthetic considerations for bariatric surgery. Anesth Analg 2002; 95: 1793–805.
Sprung J, Whalley DG, Falcone T et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg 2003; 97: 268–74.
Christou NV, Jarand J, Sylvestre JL et al. Analysis of the incidence and risk factors for wound infections in open bariatric surgery. Obes Surg 2004; 14: 16–22.
Schwartz ML, Drew RL, Chasin–Caldie M. Factors determining conversion from laparoscopic to open Roux–en–Y gastric bypass. Obes Surg 2004; 14: 1193–7.
Dresel A, Kuhn JA, McCart TM. Laparoscopic Rouxen– Y gastric bypass in morbidly obese and super morbidly obese patients. Am J Surg 2004; 187:230–2.
Taylor JD, Leitman M, Hon P et al. Outcome and complications of gastric bypass in super-super obesity versus morbid obesity.
Artuso D, Wayne M, Kaul A et al. Extremely high body mass index is not a contraindication to laparo- scopic gastric bypass. Obes Surg 2004; 14: 750–4.
Scopinaro N, Gianetta E, Adami GF et al. Biliopancreatic diversion for obesity at eighteen years. Surgery 1996; 119: 261–8.
Hess DS, Hess DW, Oakley RS. The biliopancreática diversion with the duodenal switch: Results beyond 10 years. Obes Surg 2005; 15: 408–16.
Marceau P, Hould F-S, Potvin M et al. Biliopancreatic diversion with duodenal switch procedure. In: Deitel M, ed. Update. Surgery for Morbidly Obese Patient. Toronto: FD-Communications 2000: 259–76.
Rabkin RA. The duodenal switch as an increasing and highly effective operation for morbid obesity. Obes Surg 2004; 14: 861–5.
Milone L, Strong V, Gagner M. Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI>50). Obes Surg 2005; 15: 612–7.
Almogy G, Crookes PF, Anthone GJ. Longitudinal gastrectomy as a treatment for the high-risk superobese patient. Obes Surg 2004; 14: 492–7.
Doucet E, St–Pierre S, Almeras N et al. Reduction of visceral adipose tissue during weight loss. Eur J Clin Nutr 2002; 56: 297–304.
Busseto L, Tregnaghi A, Bussolotto M et al. Visceral fat loss evaluated by total body magnetic resonance imaging in obese women operated with laparoscopic adjustable silicone gastric banding. Int J Obes 2000; 24: 60–9.
Phillips ML, Lewis MC, Chew V et al. The early effects of weight loss surgery on regional adiposity. Obes Surg 2005; 15: 1449–55.
Ross R, Rissanen J. Mobilization of visceral and subcutaneous adipose tissue in response to energy restriction and exercise. Am J Clin Nutr 1994; 60: 695–703.
Doldi SB, Micheletto G, Perrini MN et al. Treatment of morbid obesity with intragastric balloon in association with diet. Obes Surg 2002; 12: 583–7.
Liu RC, Sabnis AA, Forsyth C. The effects of acute preoperative weight loss on laparoscopic Roux–en–Y gastric bypass. Obes Surg 2005; 15: 1396–402.
Fris RJ. Preoperative low energy diet diminishes liver size. Obes Surg 2004; 14: 1165–70.
Lewis MC, Phillips ML, Slavotinek JP. Change in liver size and fat content after treatment with Optifast® very low calorie diet. Obes Surg 2006; 16: 697–701.
Genco A, Bruni T, Doldi SB et al. Bioenterics intragastric balloon: The Italian experience with 2,515 patients. Obes Surg 2005; 15: 1161–4.
Al–Momen A, El–Mogy I. Intragastric balloon for obesity: A retrospective evaluation of tolerance and efficacy. Obes Surg 2005; 15: 101–5.
Nijhof HW, Steenvoord P, Tollenaar RAEM. Perforation of the esophagus caused by the insertion of an intragastric balloon for the treatment of obesity. Obes Surg 2006; 16: 667–70.
Weiner R, Gutberlet H, Bockhorn H. Preparation of extremely obese patients for laparoscopic gastric banding by gastric-balloon therapy. Obes Surg 1999; 9: 261–4.
Busseto L, Tregnaghi A, De Marchi F et al. Liver volume and visceral obesity in women with hepatic steatosis undergoing gastric banding. Obes Res 2002; 10: 408–11.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frutos, M.D., Morales, M.D., Luján, J. et al. Intragastric Balloon Reduces Liver Volume in Super-Obese Patients, Facilitating Subsequent Laparoscopic Gastric Bypass. OBES SURG 17, 150–154 (2007). https://doi.org/10.1007/s11695-007-9040-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9040-3