Abstract
Clinical trials evaluating low molecular weight heparin (LMWH) for the prevention and treatment of venous thromboembolism and acute coronary syndromes have led to their regulatory approval for these indications in the general population. However, certain patient populations have been excluded from these landmark clinical trials, including patients with renal insufficiency, obese patients and pregnant women. In these special populations, data on safety and efficacy is limited and typically based on pharmacokinetic studies often performed in healthy subjects, or small cohort studies which are generally not powered to evaluate clinical outcomes such as bleeding or recurrent thrombosis. Because LMWH is mainly cleared renally, patients with severe renal insufficiency are at risk of LMWH accumulation and increased bleeding risks. In obese patients, there is concern regarding possible overdosing of therapeutic dose LMWH, since LMWH does not distribute in fat tissue. There are also concerns about possible underdosing of prophylactic dose LMWH in obese individuals using the standard fixed doses, particularly in the extremely obese individuals undergoing bariatric surgery. Last, pregnancy poses challenges with regards to the safety of LMWH during pregnancy and use of LMWH around delivery. This review summarizes the existing data in these special populations and proposes general recommendations for practice.
Similar content being viewed by others
References
van Dongen CJ, van den Belt AG, Prins MH, Lensing AW: Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane. Database. Syst. Rev. 2004, CD001100
Simonneau G, Sors H, Charbonnier B, Page Y, Laaban JP, Azarian R, Laurent M, Hirsch JL, Ferrari E, Mottier D, Beau B (1997) A comparison of low-molecular-weight heparin with unfractionated heparin for acute pulmonary embolism. N Engl J Med 337:663–669
Quinlan DJ, McQuillan A, Eikenboom JW (2004) Low-molecular-weight heparin compared with intravenous unfractionated heparin for treatment of pulmonary embolism. Ann Intern Med 140:175–183
Koopman MM, Prandoni P, Piovella F, Ockelford PA, Brandjes DP, van der Meer J, Gallus AS, Simonneau G, Chesterman CH, Prins MH (1996) Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. N Engl J Med 334:682–687
Schraibman IG, Milne AA, Royle EM (2001) Home versus in-patient treatment for deep vein thrombosis. Nurs Times 97:35
Levine MN, Planes A, Hirsh J, Goodyear M, Vochelle N, Gent M (1989) The relationship between anti-factor Xa level and clinical outcome in patients receiving enoxaparine low molecular weight heparin to prevent deep vein thrombosis after hip replacement. Thromb Haemost 62:940–944
Nieuwenhuis HK, Albada J, Banga JD, Sixma JJ (1991) Identification of risk factors for bleeding during treatment of acute venous thromboembolism with heparin or low molecular weight heparin. Blood 78:2337–2343
Bara L, Leizorovicz A, Picolet H, Samama M (1992) Correlation between anti-Xa and occurrence of thrombosis and haemorrhage in post-surgical patients treated with either Logiparin (LMWH) or unfractionated heparin. Post-surgery Logiparin study group. Thromb Res 65:641–650
Prandoni P, Lensing AW, Buller HR, Carta M, Cogo A, Vigo M, Casara D, Ruol A, ten Cate JW (1992) Comparison of subcutaneous low-molecular-weight heparin with intravenous standard heparin in proximal deep-vein thrombosis. Lancet 339:441–445
Walenga JM, Hoppensteadt D, Fareed J (1991) Laboratory monitoring of the clinical effects of low molecular weight heparins. Thromb Res Suppl 14:49–62
Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI (2008) Parenteral anticoagulants: American college of chest physicians evidence-based clinical practice guidelines (8th edn). Chest 133:141S–159S
Kidney Disease Outcome Quality Initiative (2002) K/DOQI clinical practice guidelines for chronic renal disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–S46
Lim W, Dentali F, Eikelboom JW, Crowther MA (2006) Meta-analysis: low-molecular-weight heparin and bleeding in patients with severe renal insufficiency. Ann Intern Med 144:673–684
Landefeld CS, Beyth RJ (1993) Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Am J Med 95:315–328
Douketis J, Cook D, Meade M, Guyatt G, Geerts W, Skrobik Y, Albert M, Granton J, Hebert P, Pagliarello G, Marshall J, Fowler R, Freitag A, Rabbat C, Anderson D, Zytaruk N, Heels-Ansdell D, Crowther M (2008) Prophylaxis against deep vein thrombosis in critically ill patients with severe renal insufficiency with the low-molecular-weight heparin dalteparin: an assessment of safety and pharmacodynamics: the DIRECT study. Arch Intern Med 168:1805–1812
Mahe I, Aghassarian M, Drouet L, Dit-Sollier CB, Lacut K, Heilmann JJ, Mottier D, Bergmann JF (2007) Tinzaparin and enoxaparin given at prophylactic dose for eight days in medical elderly patients with impaired renal function: a comparative pharmacokinetic study. Thromb Haemost 97:581–586
Tincani E, Mannucci C, Casolari B, Turrini F, Crowther MA, Prisco D, Cenci AM, Bondi M (2006) Safety of dalteparin for the prophylaxis of venous thromboembolism in elderly medical patients with renal insufficiency: a pilot study. Haematologica 91:976–979
Falga C, Capdevila JA, Soler S, Rabunal R, Sanchez Munoz-Torrero JF, Gallego P, Monreal M (2007) Clinical outcome of patients with venous thromboembolism and renal insufficiency. Findings from the RIETE registry. Thromb Haemost 98:771–776
Santopinto JJ, Fox KA, Goldberg RJ, Budaj A, Pinero G, Avezum A, Gulba D, Esteban J, Gore JM, Johnson J, Gurfinkel EP (2003) Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart 89:1003–1008
Collet JP, Montalescot G, Agnelli G, Van de WF, Gurfinkel EP, Lopez-Sendon J, Laufenberg CV, Klutman M, Gowda N, Gulba D (2005) Non-ST-segment elevation acute coronary syndrome in patients with renal dysfunction: benefit of low-molecular-weight heparin alone or with glycoprotein IIb/IIIa inhibitors on outcomes. The global registry of acute coronary events. Eur Heart J 26:2285–2293
Spinler SA, Inverso SM, Cohen M, Goodman SG, Stringer KA, Antimann EM (2003) Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J 146:33–41
Spinler SA, Mahaffey KW, Gallup D, Levine GN, Ferguson JJ III, Rao SV, Gallo R, Ducas J, Goodman SG, Antman E, White HD, Biasucci L, Becker RC, Col JJ, Cohen M, Harrington RA, Califf RM (2009) Relationship between renal function and outcomes in high-risk patients with non-ST-segment elevation acute coronary syndromes: results from SYNERGY. Int J Cardiol 2009 [Epub ahead of print]
Siguret V, Pautas E, Fevrier M, Wipff C, Durand-Gasselin B, Laurent M, Andreux JP, d’Urso M, Gaussem P (2000) Elderly patients treated with tinzaparin (Innohep) administered once daily (175 anti-Xa IU/kg): anti-Xa and anti-IIa activities over 10 days. Thromb Haemost 84:800–804
Pautas E, Gouin I, Bellot O, Andreux J-P, Siguret V (2002) Safety profile of tinzaparin administered once daily at a standard curative dose in two hundred very elderly patients. Drug Saf 25:725–733
Aventis Pharma Inc. (2004) Lovenox product monograph (enoxaparin sodium). Ref Type: Pamphlet
Fox KA, Antman EM, Montalescot G, Agewall S, SomaRaju B, Verheugt FW, Lopez-Sendon J, Hod H, Murphy SA, Braunwald E (2007) The impact of renal dysfunction on outcomes in the ExTRACT-TIMI 25 trial. J Am Coll Cardiol 49:2249–2255
Lachish T, Rudensky B, Slotki I, Zevin S (2007) Enoxaparin dosage adjustment in patients with severe renal failure: antifactor xa concentrations and safety. Pharmacotherapy 27:1347–1352
Wilson SJ, Wilbur K, Burton E, Anderson DR (2001) Effect of patient weight on the anticoagulant response to adjusted therapeutic dosage of low-molecular-weight heparin for the treatment of venous thromboembolism. Haemostasis 31:42–48
Sanderink GJ, Le Liboux A, Jariwala N, Harding N, Ozoux ML, Shukla U, Montay G, Boutouyrie B, Miro A (2002) The pharmacokinetics and pharmacodynamics of enoxaparin in obese volunteers. Clin Pharmacol Ther 72:308–318
Hainer JW, Barrett JS, Assaid CA, Fossler MJ, Cox DS, Leathers T, Leese PT (2002) Dosing in heavy-weight/obese patients with the LMWH, tinzaparin: a pharmacodynamic study. Thromb Haemost 87:817–823
Bazinet A, Almanric K, Brunet C, Turcotte I, Martineau J, Caron S, Blais N, Lalonde L (2005) Dosage of enoxaparin among obese and renal impairment patients. Thromb Res 116:41–50
Al Yaseen E, Wells PS, Anderson J, Martin J, Kovacs MJ (2005) The safety of dosing dalteparin based on actual body weight for the treatment of acute venous thromboembolism in obese patients. J Thromb Haemost 3:100–102
Barba R, Marco J, Martin-Alvarez H, Rondon P, Fernandez-Capitan C, Garcia-Bragado F, Monreal M (2005) The influence of extreme body weight on clinical outcome of patients with venous thromboembolism: findings from a prospective registry (RIETE). J Thromb Haemost 3:856–862
Mahaffey KW, Tonev ST, Spinler SA, Levine GN, Gallo R, Ducas J, Goodman SG, Antman EM, Becker RC, Langer A, White HD, Aylward PE, Col JJ, Ferguson JJ, Califf RM (2008) Obesity in patients with non-ST-segment elevation acute coronary syndromes: Results from the SYNERGY trial. Int J Cardiol
Alikhan R, Cohen AT, Combe S, Samama MM, Desjardins L, Eldor A, Janbon C, Leizorovicz A, Olsson CG, Turpie AG (2003) Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Fibrinolysis 14:341–346
Kucher N, Leizorovicz A, Vaitkus PT, Cohen AT, Turpie AG, Olsson CG, Goldhaber SZ (2005) Efficacy and safety of fixed low-dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med 165:341–345
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW (2008) Prevention of venous thromboembolism: American college of chest physicians evidence-based clinical practice guidelines (8th edn). Chest 133:381S–453S
Mason EE, Tang S, Renquist KE, Barnes DT, Cullen JJ, Doherty C, Maher JW (1997) A decade of change in obesity surgery. National bariatric surgery registry (NBSR) contributors. Obes Surg 7:189–197
White RH, Zhou H, Romano PS (2003) Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost 90:446–455
Scholten DJ, Hoedema RM, Scholten SE (2002) A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 12:19–24
Borkgren-Okonek MJ, Hart RW, Pantano JE, Rantis PC Jr, Guske PJ, Kane JM Jr, Gordon N, Sambol NC (2008) Enoxaparin thromboprophylaxis in gastric bypass patients: extended duration, dose stratification, and antifactor Xa activity. Surg Obes Relat Dis 4:625–631
Raftopoulos I, Martindale C, Cronin A, Steinberg J (2008) The effect of extended post-discharge chemical thromboprophylaxis on venous thromboembolism rates after bariatric surgery: a prospective comparison trial. Surg Endosc 22:2384–2391
Bates SM, Greer IA, Pabinger I, Sofaer S, Hirsh J (2008) Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American college of chest physicians evidence-based clinical practice guidelines (8th edn). Chest 133:844S–886S
Carlin AJ, Farquharson RG, Quenby SM, Topping J, Fraser WD (2004) Prospective observational study of bone mineral density during pregnancy: low molecular weight heparin versus control. Hum Reprod 19:1211–1214
Greer IA, Nelson-Piercy C (2005) Low-molecular-weight heparins for thromboprophylaxis and treatment of venous thromboembolism in pregnancy: a systematic review of safety and efficacy. Blood 106:401–407
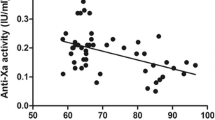
Barbour LA, Smith JM, Marlar RA (1995) Heparin levels to guide thromboembolism prophylaxis during pregnancy. Am J Obstet Gynecol 173:1869–1873
Jacobsen AF, Qvigstad E, Sandset PM (2003) Low molecular weight heparin (dalteparin) for the treatment of venous thromboembolism in pregnancy. BJOG 110:139–144
Rodie VA, Thomson AJ, Stewart FM, Quinn AJ, Walker ID, Greer IA (2002) Low molecular weight heparin for the treatment of venous thromboembolism in pregnancy: a case series. BJOG 109:1020–1024
Acknowledgments
No funding was received for the preparation of this manuscript. WL has received an unrestricted educational grant from Leo Pharma, and is on the speaker’s bureau for Leo Pharma and Pfizer and has received honoraria for these presentations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, W. Using low molecular weight heparin in special patient populations. J Thromb Thrombolysis 29, 233–240 (2010). https://doi.org/10.1007/s11239-009-0418-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-009-0418-z