Abstract
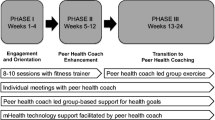
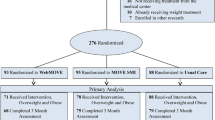
Effective and scalable lifestyle interventions are needed to address high rates of obesity in people with serious mental illness (SMI). This pilot study evaluated the feasibility of a behavioral weight loss intervention enhanced with peer support and mobile health (mHealth) technology for obese individuals with SMI. The Diabetes Prevention Program Group Lifestyle Balance intervention enhanced with peer support and mHealth technology was implemented in a community mental health setting. Thirteen obese individuals with SMI participated in a pre-post pilot study of the 24-week intervention. Feasibility was assessed by program attendance, and participant satisfaction and suggestions for improving the model. Descriptive changes in weight and fitness were also explored. Overall attendance amounted to approximately half (56 %) of weekly sessions. At 6-month follow-up, 45 % of participants had lost weight, and 45 % showed improved fitness by increasing their walking distance. Participants suggested a number of modifications to increase the relevance of the intervention for people with SMI, including less didactic instruction and more active learning, a simplified dietary component, more in depth technology training, and greater attention to mental health. The principles of standard behavioral weight loss treatment provide a useful starting point for promoting weight loss in people with SMI. However, adaptions to standard weight loss curricula are needed to enhance engagement, participation, and outcomes to respond to the unique challenges of individuals with SMI.
Similar content being viewed by others
References
Scott D, Happell B: The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues in Mental Health Nursing 32:589–597, 2011
Manu P, Dima L, Shulman M, Vancampfort D, De Hert M, Correll CU: Weight gain and obesity in schizophrenia: epidemiology, pathobiology, and management. Acta Psychiatrica Scandinavica, 2015. doi:10.1111/acps.12445.
Laursen TM, Nordentoft M, Mortensen PB: Excess early mortality in schizophrenia. Annual Review of Clinical Psychology 10:425–448, 2014. doi:10.1146/annurev-clinpsy-032813-153657
Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe R, et al.: Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. The American Journal of Psychiatry 172:344–352, 2015. doi:10.1176/appi.ajp.2014.14030357
Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, et al: A behavioral weight-loss intervention in persons with serious mental illness. The New England Journal of Medicine 368:1594–1602, 2013. doi:10.1056/NEJMoa1214530
Yarborough BJ, Stumbo SP, Yarborough MT, Young TJ, Green CA. Improving Lifestyle Interventions for People With Serious Mental Illnesses: Qualitative Results From the STRIDE Study. Psychiatric Rehabilitation Journal, 2015. doi:10.1037/prj0000151.
Aschbrenner K, Carpenter-Song E, Mueser K, Kinney A, Pratt S, Bartels S: A qualitative study of social facilitators and barriers to health behavior change among persons with serious mental illness. Community Mental Health Journal 49:207–212, 2013. doi:10.1007/s10597-012-9552-8.
Venditti EM, Kramer MK: Diabetes Prevention Program Community Outreach Perspectives on Lifestyle Training and Translation. American Journal of Preventive Medicine 44:S339–S345, 2013. doi:10.1016/j.amepre.2012.12.014.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al.: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine 346:393–403, 2002. doi:10.1056/NEJMoa012512.
Ali MK, Echouffo-Tcheugui J, Williamson DF: How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health affairs (Project Hope). 31:67–75, 2012. doi:10.1377/hlthaff.2011.1009.
Piette JD, Resnicow K, Choi H, Heisler M: A diabetes peer support intervention that improved glycemic control: mediators and moderators of intervention effectiveness. Chronic Illness 9:258–267, 2013. doi:10.1177/1742395313476522.
Moskowitz D, Thom DH, Hessler D, Ghorob A, Bodenheimer T: Peer coaching to improve diabetes self-management: which patients benefit most? Journal of General Internal Medicine 28:938–942, 2013. doi:10.1007/s11606-013-2367-7.
Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, et al.: The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia Research 118:264–270, 2010. doi:10.1016/j.schres.2010.01.026.
Leahey TM, Kumar R, Weinberg BM, Wing RR: Teammates and social influence affect weight loss outcomes in a team-based weight loss competition. Obesity (Silver Spring, Md) 20:1413–1418, 2012. doi:10.1038/oby.2012.18.
Leahey TM, Wing RR: A randomized controlled pilot study testing three types of health coaches for obesity treatment: Professional, peer, and mentor. Obesity (Silver Spring, Md) 21:928–934, 2013. doi:10.1002/oby.20271; 10.1038/oby.2012.179.
Aschbrenner K, Naslund J, Barre L, Mueser K, Kinney A, Bartels S. Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Translational Behavioral Medicine 1–8, 2015. doi:10.1007/s13142-015-0313-4.
Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE: Mobile technologies among people with serious mental illness: opportunities for future services. Administration and Policy in Mental Health 40:340–343, 2013. doi:10.1007/s10488-012-0424-x.
Hidalgo-Mazzei D, Mateu A, Reinares M, Undurraga J, Bonnin Cdel M, Sanchez-Moreno J. et al.: Self-monitoring and psychoeducation in bipolar patients with a smart-phone application (SIMPLe) project: Design, development and studies protocols. BMC Psychiatry 15:52, 2015. doi:10.1186/s12888-015-0437-6.
Faurholt-Jepsen M, Vinberg M, Frost M, Christensen EM, Bardram J, Kessing LV: Daily electronic monitoring of subjective and objective measures of illness activity in bipolar disorder using smartphones–the MONARCA II trial protocol: A randomized controlled single-blind parallel-group trial. BMC Psychiatry 14:309, 2014. doi:10.1186/s12888-014-0309-5.
Alvarez-Jimenez M, Alcazar-Corcoles MA, Gonzalez-Blanch C, Bendall S, McGorry PD, Gleeson JF: Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophrenia Research 156:96–106, 2014. doi:10.1016/j.schres.2014.03.021.
Naslund JA, Marsch LA, McHugo GJ, Bartels SJ: Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health (Abingdon, England) 1–12, 2015. doi:10.3109/09638237.2015.1019054.
Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ: Feasibility of popular m-Health technologies for activity tracking among individuals with serious mental illness. Telemedicine and e-Health 21:213–216, 2015. doi:10.1089/tmj.2014.0105.
Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M: Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science: A Journal of the Association for Psychological Science 2:22–34, 2014. doi:10.1177/2167702613497932.
Folstein MF, Folstein SE, McHugh PR: Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189–198, 1975.
Zhang W: Mixed methods application in health intervention research: A multiple case study. International Journal of Multiple Research Approaches 8:24–35, 2014. doi:10.5172/mra.2014.8.1.24.
Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al.: Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. The American Journal of Preventive Medicine 37:505–511, 2009. doi:10.1016/j.amepre.2009.07.020.
Naslund JA, Aschbrenner K, Bartels S: Acceptability of Facebook for Health Promotion in People with Serious Mental Illness. Under Review.
Meyer PS, Johnson DP, Parks A, Iwanski C, Penn DL: Positive living: A pilot study of group positive psychotherapy for people with schizophrenia. The Journal of Positive Psychology 7:239–248, 2012. doi:10.1080/17439760.2012.677467.
Balke B. A SIMPLE FIELD TEST FOR THE ASSESSMENT OF PHYSICAL FITNESS. REP 63-6. [Report] Civil Aeromedical Research Institute (US) 1–8, 1963.
Larsson UE, Reynisdottir S: The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiotherapy Research International : The Journal for Researchers and Clinicians in Physical Therapy 13:84–93, 2008. doi:10.1002/pri.398.
Beriault K, Carpentier AC, Gagnon C, Menard J, Baillargeon JP, Ardilouze JL, et al: Reproducibility of the 6-minute walk test in obese adults. International Journal of Sports Medicine 30:725–727, 2009. doi:10.1055/s-0029-1231043.
Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, et al.: Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. JAMA 270:1702–1707, 1993.
Braun V, Clarke V: Using thematic analysis in psychology. Qualitative Research in Psychology 3:77–101, 2006. doi:10.1191/1478088706qp063oa.
Solomon P: Rapid assessment of existing HIV prevention programming in a community mental health center. Journal of Prevention & Intervention in the Community 33:137–151, 2007.
Beebe J: Rapid Assessment Process. Walnut Cree, Altamira Press, 2001.
Schneider KL, Sullivan JC, Pagoto SL: Translation of the diabetes prevention program into a community mental health organization for individuals with severe mental illness: a case study. Translational behavioral medicine 1:453–460, 2011. doi:10.1007/s13142-011-0053-z.
Srebnik D, Chwastiak LA, Russo J, Sylla L: A pilot study of the diabetes prevention program on weight loss for adults at community mental health centers. Psychiatric Services (Wash, DC) 66:200-203, 2015. doi:10.1176/appi.ps.201300576.
Trivedi JK: Cognitive deficits in psychiatric disorders: Current status. Indian Journal of Psychiatry 48:10–20, 2006. doi:10.4103/0019-5545.31613.
Bandura A: Health promotion from the perspective of social cognitive theory. Psychology and health 13:623–649, 1998.
Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, et al.: Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Medicine 13:84, 2015. doi:10.1186/s12916-015-0323-6.
Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, et al.: Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric services (Wash, DC) 64:729–736, 2013. doi:10.1176/appi.ps.003622012.
Burke LE, Wang J, Sevick MA: Self-monitoring in weight loss: A systematic review of the literature. Journal of the American Dietetic Association 111:92–102, 2011. doi:10.1016/j.jada.2010.10.008.
Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. The Cochrane Database of Systematic Reviews 4:Cd004366, 2008. doi:10.1002/14651858.CD004366.pub3.
Anderson E, Shivakumar G: Effects of exercise and physical activity on anxiety. Frontiers in Psychiatry 4:27, 2013
Pinto Pereira SM, Geoffroy MC, Power C: Depressive symptoms and physical activity during 3 decades in adult life: bidirectional associations in a prospective cohort study. JAMA Psychiatry 71:1373–1380, 2014.
Naslund JA, Aschbrenner K, Bartels S: Wearable mHealth Activity Tracking for Health Promotion in People with Serious Mental Illness: Using Participant Feedback to Inform Future Interventions. Under Review.
Ben-Zeev D, Kaiser SM, Krzos I: Remote “hovering” with individuals with psychotic disorders and substance use: feasibility, engagement, and therapeutic alliance with a text-messaging mobile interventionist. Journal of Dual Diagnosis 10:197–203, 2014. doi:10.1080/15504263.2014.962336
Leon AC, Davis LL, Kraemer HC: The Role and Interpretation of Pilot Studies in Clinical Research. Journal of Psychiatric Research 45:626–629, 2011. doi:10.1016/j.jpsychires.2010.10.008
Acknowledgments
The authors wish to think Stacey Zawacki, DrPH, RDN, for expert consultation on the nutrition component of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflict of interest as it relates to the subject of this manuscript.
Funding
This study was supported by an AHRQ funded K12 Career Development Fellowship for Patient-Centered Outcomes Research awarded to the first author (K12 HS021695-01, PI: Bartels). Additional support was received from the United States Centers for Disease Control and Prevention Health Promotion and Disease Prevention Research Center (Cooperative Agreement Number U48DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Aschbrenner, K.A., Naslund, J.A., Shevenell, M. et al. Feasibility of Behavioral Weight Loss Treatment Enhanced with Peer Support and Mobile Health Technology for Individuals with Serious Mental Illness. Psychiatr Q 87, 401–415 (2016). https://doi.org/10.1007/s11126-015-9395-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-015-9395-x