Abstract
Glucagon-like Peptide-1 receptor agonists (GLP1-ra) are a relatively new class of anti-hyperglycemic drugs which may positively affect bone metabolism and thereby decrease (osteoporotic) bone fracture risk. Data on the effect of GLP1-ra on fracture risk are scarce and limited to clinical trial data only. The aim of this study was to investigate, in a population-based cohort, the association between the use of GLP1-ra and bone fracture risk. We conducted a population-based cohort study, with the use of data from the Clinical Practice Research Datalink (CPRD) database (2007–2012). The study population (N = 216,816) consisted of all individuals with type 2 diabetes patients with at least one prescription for a non-insulin anti-diabetic drug and were over 18 years of age. Cox proportional hazards models were used to estimate the hazard ratio of fracture in GLP1-ra users versus never-GLP1-ra users. Time-dependent adjustments were made for age, sex, lifestyle, comorbidity and the use of other drugs. There was no decreased risk of fracture with current use of GLP1-ra compared to never-GLP1-ra use (adjusted HR 0.99, 95 % CI 0.82–1.19). Osteoporotic fracture risk was also not decreased by current GLP1-ra use (adjusted HR 0.97; 95 % CI 0.72–1.32). In addition, stratification according to cumulative dose did not show a decreased bone fracture risk with increasing cumulative GLP1-ra dose. We showed in a population-based cohort study that GLP1-ra use is not associated with a decreased bone fracture risk compared to users of other anti-hyperglycemic drugs. Future research is needed to elucidate the potential working mechanisms of GLP1-ra on bone.
Similar content being viewed by others
Introduction
In individuals with type 2 diabetes, the risk of bone fracture is increased compared to individuals without type 2 diabetes [1]. This increased risk might be associated with the pathobiology of type 2 diabetes itself, although the underlying mechanisms remain largely unknown [2]. Alternatively, it has been suggested that this increased bone fracture risk is a consequence of the kind of therapeutic regimen initiated to combat hyperglycemia [3]. For instance, thiazolidinediones [4–6] have shown to increase fracture risk. It has been suggested that human recombinant insulins [7] also increase bone fracture risk, whereas metformin might actually decrease it [8].
Glucagon-like peptide-1 receptor agonists (GLP1-ra) are a relative new class of anti-hyperglycemic drugs, which may positively affect bone metabolism [9–11] and decrease bone fracture risk. However, a recent meta-analysis, based upon randomized clinical trial data, in which bone fractures were not a primary outcome, did not show a decreased bone fracture risk [12]. Thus, the aim of the present study was to investigate, in a large population-based cohort study, the association between GLP1-ra use and the risk of bone fractures in individuals with type 2 diabetes.
Methods
Data Source
Data were obtained from the British Clinical Practice Research Datalink [CPRD; previously the General Practice Research Database (GPRD); see (www.CPRD.com)]. The CPRD contains computerized medical records of 625 primary care practices in the United Kingdom (UK), and patients represent 8 % of the UK population. Data have been collected since 1987 and include, amongst others, demographic information, prescription details, data on morbidity and mortality, preventive care provided and specialist referrals. Data in the CPRD have been shown to be accurate and valid [13]. Particularly, with regard to the main outcome of the present study, fractures have been validated in over 90 % of all cases [14].
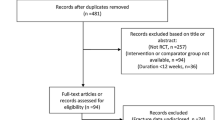
Study Population
We conducted a population-based cohort study. The population consisted of all patients with at least one prescription for a non-insulin anti-hyperglycemic drug (NIAD) and who were aged 18+ during the period of valid CPRD data collection [15]. Cohort entry was defined as the date of first prescription for GLP1-ra, identified between June 13th, 2007 and August 31, 2012. The index date was defined as the date of the first NIAD prescription; thereby the study population was a mix of incident and prevalent NIAD users. Patients were followed from the index date to the end of data collection, date of transfer of the patient out of the practice area, patient’s death, or fracture types of interest, whichever came first.
Exposure
Follow-up time was divided into intervals based on NIAD and insulin prescriptions. Thus a new interval was created for every prescription. When there was a washout period of 90 days, an interval was classified as “past use”, until end of follow-up, or a new anti-hyperglycemic drug prescription, whichever came first. In all other circumstances, an interval was classified as “current use”. If no GLP1-ra was prescribed during follow-up, person-time was classified as never use of GLP1-ra.
All GLP1-ra exposed intervals were classified, according to the time since the most recent prescription, as current (1–90 days), recent (91–180 days), or past (over 180 days) GLP1-ra use. At every current use interval, the cumulative prescribed GLP1-ra dosage, in exenatide dose equivalents, was reviewed and divided by the GLP1-ra treatment time (difference in time between the start of the first and last GLP1-ra prescription) to estimate the average daily GLP1-ra dose. Defined daily doses were used to calculate the exenatide dose equivalents [16].
Outcomes
Patients were followed from the index date to the end of data collection, date of transfer of the patient out of the practice area, patient’s death, or fracture types of interest, whichever came first. Fractures were classified with the use of READ codes [17] into hip, radius and (or) ulna, vertebral, humerus and other fractures. A major osteoporotic fracture was defined according to the WHO definition as a fracture of the hip, humerus, vertebral or radius/ulna [18].
Other Variables
The presence of risk factors for bone fractures was assessed by reviewing the computerized medical records for any record of any risk factors for bone fractures prior to the start of an interval. The following potential confounders were determined at baseline: sex, body mass index (BMI), smoking status and alcohol use. All other potential confounders that were considered in this study were determined time-dependent (i.e. at the start of each interval): age, falls in 7–12 months before the start of an interval, a history of chronic obstructive pulmonary disease (COPD), a previous fracture, rheumatoid arthritis, hypothyroidism, hyperthyroidism, cancer, retinopathy, neuropathy, secondary osteoporosis (hypogonadism or early menopause) and congestive heart failure. The most recent HbA1c value up to 1 year prior to the start of an interval was determined. The following drug prescriptions, in the 6 months prior to the start of an interval, were considered potential confounders; oral glucocorticoids [19], cholesterol lowering drugs, antidepressants [20], anxiolytics or hypnotics [21], antipsychotics, anti-Parkinson drugs [22], antihypertensives (beta-blockers, thiazide diuretics, renin-angiotensin-aldosterone-system (RAAS) inhibitors, calcium channel blockers and loop diuretics), antiarrhythmics, hormone replacement therapy, calcium, bisphosphonates, vitamin D, raloxifene, strontium ranelate, calcitonin and parathyroid hormone.
Statistical Analyses
Regression analysis with Cox proportional hazards models (SAS 9.2, PHREG procedure) was used to estimate bone fracture risk of GLP1-ra users (current, recent or past) compared to never-GLP1-ra users. Current GLP1-ra use was further stratified to age and gender, and the main analyses were repeated for major osteoporotic bone fracture risk. In a series of further analyses, current GLP1-ra use was stratified according to type of GLP1-ra (i.e. exenatide and liraglutide), daily and cumulative dose. As a sensitivity analysis, the person-time for thiazolidinediones (TZD) was excluded from the reference group and analysed as a separate group.
In all analyses, potential confounders were included if they independently changed the beta-coefficient for current GLP1-ra exposure by at least 5 %, or when consensus about inclusion existed within the team of researchers, supported by clinical evidence from the literature.
Results
Study Population and Follow-up
In total, 216,816 individuals were included in the present study, of which 8,354 used GLP1-ra (either current, recent or past). The characteristics of the study population are presented in Table 1. On average, GLP1-ra users were younger than never-GLP1-ra users (53.5 vs. 61.0 years), and had a higher BMI (37.5 vs. 31.0). The median duration of follow-up time (from start of follow-up to end of data collection) was 5.1 years [Interquartile Range (IQR): 3.6–5.2 years] for GLP1-ra users and 3.6 years [IQR: 1.6–5.2 years] for never-GLP1-ra users.
Current, Recent or Past GLP1-ra Use and the Risk of Bone Fracture
After adjusting for confounders, the risk for bone fractures with current GLP1-ra, compared to never-GLP1-ra users, was [Hazard Ratio (HR) and (95 %CI)] 0.99 (0.82–1.19), with recent GLP1-ra use: 1.19 (0.66–2.14) and with past GLP1-ra use: 1.38 (1.03–1.84), Table 2. Stratification of current GLP1-ra by GLP1-ra type resulted in an adjusted (adj.) HR of 0.90 (0.69–1.17) with use of liraglutide and an adj. HR of 1.08 (0.84–1.38) with exenatide use.
When stratified by sex, bone fracture risk for current male GLP1-ra users was 1.01 (0.76–1.33) and for current female GLP1-ra users was 0.96 (0.75–1.22), Table 2. After stratification by age group (i.e. 18–49, 50–59, 60–69 and ≥70 years), the risk for bone fractures among patients with current GLP1-ra use aged 18–49 was 0.80 (0.52–1.25), aged 50–59 was 0.80 (0.56–1.15), aged 60–69 was 1.38 (1.04–1.83) and aged 70 years or older was 0.68 (0.39–1.18), Table 2.
As compared to never-GLP1-ra use, the risk for major osteoporotic fractures with current GLP1-ra use was 0.97 (0.72–1.32); with recent GLP1-ra use, 1.13 (0.42–3.02) and with past GLP1-ra use, 1.04 (0.61–1.76), Table 3, (detailed data not shown). Current GLP1-ra use was not associated with a decreased bone fracture risk for other fracture types, Table 3.
Bone Fracture Risk and Current GLP1-ra Use Stratified According to Dosage
If current GLP1-ra use was stratified according to cumulative dose (i.e. 0–2.7 mg, 2.8–5.4 mg, 5.5–8.2 mg and ≥8.3 mg exenatide dose equivalents) the results showed that, as compared to never-GLP1-ra users, bone fracture risk for 0–2.7 mg was 1.02 (95 % CI 0.75–1.40), for 2.7–5.5 mg, 0.89 (0.60–1.34); for 5.5–8.2 mg, 0.94 (0.58–1.52) and for ≥8.3 mg, 1.03 (0.75–1.41). When stratified according to current GLP1-ra average daily dose use (i.e. missing, 0–15 mcg, 16–20 mcg and >20 mcg exenatide dose equivalents), the results were not substantially altered, Table 4.
Sensitivity Analyses
As TZD use has been associated with an increased risk of fracture, we additionally excluded for the main analysis all TZD exposed person-time from the reference group and analysed it as a separate group. This did not substantially change the results of GLP1-ra use (adj. HR with current GLP1-ra use; 1.03 (0.86–1.24), with recent GLP1-ra use; 1.19 (0.66–2.15) and with past GLP1-ra use; 1.38 (1.03–1.84)).
Discussion
The results of the present population-based study show that (osteoporotic) bone fracture risk was not decreased by GLP1-ra use. In addition, stratification according to cumulative dose did not show a decreased risk of bone fracture with increasing cumulative GLP-1 dose. The results of the present study thereby do not support the hypothesis that GLP1-ra use may reduce bone fracture risk in individuals with type 2 diabetes. The results of our study add to the field population-based data and are indirectly supported by a clinical trial on the effect of exenatide on markers of bone remodelling and calcium homeostasis, which failed to show a positive effect [23]. Our study is thereby in line with a recent meta-analysis [12] done on randomized clinical trial data. Another more recent meta-analysis also showed no association between use of GLP1-ra and fracture risk [24]. However, after stratification to GLP1-ra type, they found a decreased risk of fracture with use of liraglutide and an increased risk of fracture with use of exenatide. The results of our study did not show a decreased or increased risk after stratification by GLP1-ra type. It has to be taken into account, however, that the included studies of these meta-analyses were not designed to investigate fracture risk and that fractures were not routinely registered. The results of our study are also in keeping with the results of a large cohort study on the use of dipeptidyl peptidase-4 inhibitors (DPP4-I) and fracture risk which also did not show a decreased fracture risk [25].
The pathways through which GLP1-ra’s may act on bone metabolism are not fully elucidated, but it has been suggested that GLP1-ra’s may, either directly or indirectly, shift the balance in bone homeostasis towards bone formation [26], via receptor coupling on osteoblasts [27] and (or) thyroid C cells [28, 29]. Alternatively, it has been suggested that GLP1-ra may increase calcitonin concentration [29, 30] and decrease sclerostin which both may inhibit bone formation [31]. Nevertheless, it remains to be determined whether such mechanisms may also be operative in humans. Interestingly, a recent meta-analysis of clinical trial data on the use of DPP4-I did show a 40 % reduction in the risk of bone fracture [32]. The latter brings forward the hypothesis that any effects on bone metabolism by DPP4-I might be independent from the direct effect of GLP1 on bone, despite the pharmacodynamics through which they are linked [3]. However, the underlying mechanisms between anti-hyperglycemic drug use along the GLP-1/DPP4-I axis and bone fracture risk in type 2 diabetes in humans remain complex.
Unexpectedly, our results showed a 1.4-fold increase in bone fracture risk for past GLP1-ra users (GLP1-ra use had discontinued ≥180 days) and for patients aged 60–69 compared to never-GLP1-ra users. As any plausible underlying mechanism seems missing, we consider these results as a play of chance.
Our study had several strengths. Firstly, the results were based upon population-based data that may have prevented, at least partially, selection bias as compared to randomized clinical trials in which only patients meeting specific inclusion criteria are able to participate. Secondly, bone fractures are often not primary end-points in clinical trials, thus their registration may be inadequate. The current study, however, was able to partially circumvent this potential bias, as over 90 % of all fractures have been clinically validated in the CPRD [14]. Finally, all participants were extensively clinically characterized which allowed us to take a series of potential confounders, including prior medical history, into account. In addition, we were able to adjust for neuropathy, retinopathy and HbA1c with which we tried to capture disease severity. In particular, HbA1c could act as a potential confounder of the association between GLP1-ra use and bone fracture risk in individuals with type 2 diabetes. However, it is acknowledged that some residual confounding may still be present.
When interpreting the results, a couple of limitations are worth mentioning. First, an important consideration, in light of the discussion on GLP1-ra use and bone fracture risk, in terms of time effect, is the average duration of GLP1-ra use. In our analysis, the median duration of actual GLP1-ra use was 1.2 years (from first GLP1-ra prescription until last GLP1-ra prescription), and this might be relatively short. For bisphosphonate use, it has been shown that bone fracture risk starts to decrease after 1–1.5 years of use [33, 34]. Even for the highest cumulative dose group (i.e. ≥8.3 mg), which could be equivalent to 1 DDD GLP1-ra per day during at least 1.5 years, we did not show a decrease in bone fracture risk. However, the time-window for GLP1-ra to exert an effect on bone fracture risk is not yet determined. Second, the risk of fracture is known to increase with age [35], yet we identified that patients who used GLP1-ra were slightly younger at baseline, compared to never-GLP1-ra users. Thus, this might have masked the protective effect of GLP1-ra on risk of bone fracture. Yet, our age-stratified analyses did not show a protective effect of GLP1-ra use on bone fracture risk. Third, GLP1-ra's are selectively prescribed to patients with an high BMI, which might have influenced the results. High BMI has been associated with a lower risk of fracture [36], and this might even strengthen the protective effect of GLP1-ra. However, we could not show a protective effect of GLP1-ra on fracture risk. Fourth, after stratification of the analyses to specific fracture types, the number of fractures within the current GLP1-ra group became low, and therefore, the results should be interpreted with caution.
In summary, we showed in a population-based cohort study that GLP1-ra use is not associated with a decreased risk of bone fracture as compared to users of other anti-hyperglycemic drugs. Future research is needed to elucidate the working mechanisms of the complex GLP-1/DPP-4 axis and to investigate the time-window of GLP1-ra to exert an effect on bone fracture risk.
References
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18(4):427–444
Carnevale V, Romagnoli E, D’Erasmo E (2004) Skeletal involvement in patients with diabetes mellitus. Diabetes Metab Res Rev. 20(3):196–204
Montagnani A, Gonnelli S (2013) Diabetes Obes Metab. Antidiabetic therapy effects on bone metabolism and fracture risk. 15(9):784–791
Bazelier MT, Gallagher AM, van Staa TP, Cooper C, Leufkens HG, Vestergaard P, de Vries F (2012) Use of thiazolidinediones and risk of osteoporotic fracture: disease or drugs? Pharmacoepidemiol Drug Saf 21(5):507–514
Bazelier MT, Vestergaard P, Gallagher AM, van Staa TP, Cooper C, Leufkens HG, de Vries F (2012) Risk of fracture with thiazolidinediones: disease or drugs? Calcif Tissue Int 26(9):2271–2279
Betteridge DJ (2011) Thiazolidinediones and fracture risk in patients with type 2 diabetes. Diabet Med 28(7):759–771
Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, Donaldson MG, Cauley JA, Harris TB, Koster A, Womack CR, Palermo L, Black DM (2011) Study of Osteoporotic Fractures (SOF) Research Group; Osteoporotic Fractures in Men (MrOS) Research Group; Health, Aging, and Body Composition (Health ABC) Research Group. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305(21):2184–2192
Vestergaard P, Rejnmark L, Mosekilde L (2005) Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia 48(7):1292–1299
Nuche-Berenguer B, Moreno P, Esbrit P, Dapía S, Caeiro JR, Cancelas J, Haro-Mora JJ, Villanueva-Peñacarrillo ML (2009) Effect of GLP-1 treatment on bone turnover in normal, type 2 diabetic, and insulin-resistant states. Calcif Tissue Int 84:453–461
Nuche-Berenguer B, Moreno P, Portal-Nuñez S, Dapía S, Esbrit P, Villanueva-Peñacarrillo ML (2010) Exendin-4 exerts osteogenic actions in insulin-resistant and type 2 diabetic states. Regul Pept 159(1–3):61–66
Moreno P, Nuche-Berenguer B, Gutiérrez-Rojas I, Acitores A, Sancho V, Valverde I, González N, Villanueva-Peñacarrillo ML (2012) Normalizing action of exendin-4 and GLP-1 in the glucose metabolism of extrapancreatic tissues in insulin-resistant and type 2 diabetic states. J Mol Endocrinol 48:37–47
Mabilleau G, Mieczkowska A, Chappard D (2014) Use of glucagon-like peptide-1 receptor agonists and bone fractures: a meta-analysis of randomized clinical trials. J Diabetes. 6(3):260–266
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ (2010) Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 69(1):4–14
Van Staa TP, Abenhaim L, Cooper C, Zhang B, Leufkens HG (2000) The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf 9(5):359–366
Eppenga WL, Lalmohamed A, Geerts AF, Derijks HJ, Wensing M, Egberts A et al (2014) Risk of lactic acidosis or elevated lactate concentrations in metformin users with renal impairment: a population-based cohort study. Diabetes Care 37(8):2218–2224
Anonymous. ATC classification index with DDDs (2002). Nydalen, WHO Collaborating Centre for Drug Statistics Methodology, Norwegian Institute of Public Health, 2002
Health and Social Care Information Centre: UK terminology centre-read codes. http://systems.hscic.gov.uk/data/uktc/readcodes/index_html. Accessed May 2014
FRAX. WHO Fracture Risk Assessment Tool. (2001). www.shef.ac.uk/FRAX/index.aspx. Accessed May 2014
Klop C, de Vries F, Vinks T, Kooij MJ, van Staa TP, Bijlsma JW, Egberts AC, Bouvy ML (2014) Increase in prophylaxis of glucocorticoid-induced osteoporosis by pharmacist feedback: a randomised controlled trial. Osteoporos Int 25(1):385–392
Prieto-Alhambra D, Petri H, Goldenberg JS, Khong TP, Klungel OH, Robinson NJ, de Vries F (2014) Excess risk of hip fractures attributable to the use of antidepressants in five European countries and the USA. Osteoporos Int 25(3):847–855
Khong TP, de Vries F, Goldenberg JS, Klungel OH, Robinson NJ, Ibáñez L, Petri H (2012) Potential impact of benzodiazepine use on the rate of hip fractures in five large European countries and the United States. Calcif Tissue Int 91(1):24–31
Pouwels S, Bazelier MT, de Boer A, Weber WE, Neef C, Cooper C, de Vries F (2013) Risk of fracture in patients with Parkinson’s disease. Osteoporos Int 24(8):2283–2290
Bunck MC, Eliasson B, Corner A, Heine RJ, Shaginian RM, Taskinen MR, Yki-Järvinen H, Smith U, Diamant M (2011) Exenatide treatment did not affect bone mineral density despite body weight reduction in patients with type 2 diabetes. Diabetes Obes Metab 13:374–377
Su B, Sheng H, Zhang M, Bu L, Yang P, Li L, Li F, Sheng C, Han Y, Qu S, Wang J (2015) Risk of bone fractures associated with glucagon-like peptide-1 receptor agonists’ treatment: a meta-analysis of randomized controlled trials. Endocrine 48(1):107–115
Driessen JH, van Onzenoort HA, Henry RM, Lalmohamed A, van den Bergh JP, Neef C et al (2014) Use of dipeptidyl peptidase-4 inhibitors for type 2 diabetes mellitus and risk of fracture. Bone 68:124–130
Ceccarelli E, Guarino EG, Merlotti D, Patti A, Gennari L, Nuti R, Dotta F (2013) Beyond glycemic control in diabetes mellitus: effects of incretin-based therapies on bone metabolism. Front Endocrinol (Lausanne). 18(4):73
Nuche-Berenguer B, Portal-Núñez S, Moreno P, González N, Acitores A, López-Herradón A, Esbrit P, Valverde I, Villanueva-Peñacarrillo ML (2010) Presence of a functional receptor for GLP-1 in osteoblastic cells, independent of the cAMP-linked GLP-1 receptor. J Cell Physiol 225(2):585–592
Crespel A, De Boisvilliers F, Gros L, Kervran A (1996) Effects of glucagon and glucagon-like peptide-1-(7–36) amide on C cells from rat thyroid and medullary thyroid carcinoma CA-77 cell line. Endocrinology 137(9):3674–3680
Lamari Y, Boissard C, Moukhtar MS, Jullienne A, Rosselin G, Garel JM (1996) Expression of glucagon-like peptide 1 receptor in a murine C cell line: regulation of calcitonin gene by glucagon-like peptide 1. FEBS Lett 393(2–3):248–252
Yamada C, Yamada Y, Tsukiyama K, Yamada K, Udagawa N, Takahashi N et al (2008) The murine glucagon-like peptide-1 receptor is essential for control of bone resorption. Endocrinology 149(2):547–549
Kim JY, Lee SK, Jo KJ, Song DY, Lim DM, Park KY, Bonewald LF, Kim BJ (2013) Exendin-4 increases bone mineral density in type 2 diabetic OLETF rats potentially through the down-regulation of SOST/sclerostin in osteocytes. Life Sci. 92(10):533–540
Monami M, Dicembrini I, Antenore A, Mannucci E (2011) Dipeptidyl peptidase-4 inhibitors and bone fractures: a meta-analysis of randomized clinical trials. Diabetes Care 34(11):2474–2476
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. J Am Med Assoc 280:2077–2082
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ (2001) Reginster JY; Hip Intervention Program Study Group. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340
van Staa TP, Dennison EM, Leufkens HG, Cooper C (2001) Epidemiology of fractures in England and Wales. Bone 29(6):517–522
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Acknowledgments
Andrea M. Burden is supported by a Canadian Institutes of Health Research (CIHR) Post-Doctoral Fellowship.
Conflict of Interest
Johanna H. M. Driessen, Andrea M. Burden, Hubert G. M. Leufkens and Frank de Vries declare that they are employed by the Division of Pharmacoepidemiology and Clinical Pharmacology at Utrecht Institute for Pharmaceutical Sciences, which has received unrestricted funding from the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), the Royal Dutch Pharmacists Association (KNMP), the private–public funded Top Institute Pharma (www.tipharma.nl), includes co-funding from universities, government and industry, the EU Innovative Medicines Initiative (IMI), the EU 7th Framework Program (FP7), the Dutch Ministry of Health and industry (including GlaxoSmithKline, Pfizer and others). DPA reports grants from Bioiberica, grants from Amgen Spain and an educational grant from Bioiberica, all outside the submitted work. HL is a researcher at The WHO Collaborating Centre for Pharmaceutical Policy & Regulation, which receives no direct funding or donations from private parties, including pharma industry. Research funding from public–private partnerships, e.g. IMI, TI Pharma (www.tipharma.nl), is accepted under the condition that no company-specific product or company-related study is conducted. The Centre has received unrestricted research funding from public sources, e.g. Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), EU 7th Framework Program (FP7), Dutch Medicines Evaluation Board (MEB), and Dutch Ministry of Health. Ronald M. A. Henry, Hein A. W. van Onzenoort, Arief Lalmohamed, Andrea M. Burden and Cees Neef declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Driessen, J.H.M., Henry, R.M.A., van Onzenoort, H.A.W. et al. Bone Fracture Risk is Not Associated with the Use of Glucagon-Like Peptide-1 Receptor Agonists: A Population-Based Cohort Analysis. Calcif Tissue Int 97, 104–112 (2015). https://doi.org/10.1007/s00223-015-9993-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-9993-5