Abstract
Aims/hypothesis
The aim of this prospective nationwide study was to examine antenatal pregnancy care and pregnancy outcomes in women with type 1 and type 2 diabetes, and to describe changes since 2002/2003.
Methods
This national population-based cohort included 3036 pregnant women with diabetes from 155 maternity clinics in England and Wales who delivered during 2015. The main outcome measures were maternal glycaemic control, preterm delivery (before 37 weeks), infant large for gestational age (LGA), and rates of congenital anomaly, stillbirth and neonatal death.
Results
Of 3036 women, 1563 (51%) had type 1, 1386 (46%) had type 2 and 87 (3%) had other types of diabetes. The percentage of women achieving HbA1c < 6.5% (48 mmol/mol) in early pregnancy varied greatly between clinics (median [interquartile range] 14.3% [7.7–22.2] for type 1, 37.0% [27.3–46.2] for type 2). The number of infants born preterm (21.7% vs 39.7%) and LGA (23.9% vs 46.4%) were lower for women with type 2 compared with type 1 diabetes (both p < 0.001). The prevalence rates for congenital anomaly (46.2/1000 births for type 1, 34.6/1000 births for type 2) and neonatal death (8.1/1000 births for type 1, 11.4/1000 births for type 2) were unchanged since 2002/2003. Stillbirth rates are almost 2.5 times lower than in 2002/2003 (10.7 vs 25.8/1000 births for type 1, p = 0.0012; 10.5 vs 29.2/1000 births for type 2, p = 0.0091).
Conclusions/interpretation
Stillbirth rates among women with type 1 and type 2 diabetes have decreased since 2002/2003. Rates of preterm delivery and LGA infants are lower in women with type 2 compared with type 1 diabetes. In women with type 1 diabetes, suboptimal glucose control and high rates of perinatal morbidity persist with substantial variations between clinics.
Data availability
Further details of the data collection methodology, individual clinic data and the full audit reports for healthcare professionals and service users are available from http://content.digital.nhs.uk/npid.
Similar content being viewed by others
Introduction
Pregnancy in women with diabetes is associated with increased risks of serious adverse outcomes with a two-to-five fold increased risk of congenital anomaly, stillbirth and neonatal death compared with the general maternity population [1,2,3]. Less severe but more frequent perinatal complications relating to maternal diabetes include preterm delivery, large for gestational age (LGA) infants and neonatal intensive care unit admission, affecting approximately one in two babies [4, 5]. Nationwide studies from the Netherlands, Sweden and Finland suggest no improvement in either rates of serious adverse pregnancy outcomes or perinatal complications in recent decades, with possible explanations including increasing maternal age, longer duration of diabetes and increasing rates of overweight and obesity among women of reproductive years.
A 2002/2003 population-based study, conducted by the Confidential Enquiry into Maternal and Child Health (CEMACH), examined the quality of maternity care and documented pregnancy outcomes in the UK among women with diabetes, concluding that pregnancy preparation was inadequate, resulting in potentially modifiable poor pregnancy outcomes in both type 1 and type 2 diabetes [6]. Since then the National Institute for Health and Care Excellence (NICE) have developed diabetes pregnancy guidelines with a clear emphasis on improving provision of prepregnancy and antenatal diabetes care [7]. The NICE guideline recommendations for prepregnancy preparation include taking 5 mg preconception folic acid, presenting for antenatal care before 8 weeks’ gestation and avoiding potentially harmful medications. The 2015 update lowered the maternal glycaemic control target from HbA1c < 7.0% (53 mmol/mol) to HbA1c < 6.5% (48 mmol/mol) and recommended elective delivery between 37+0 and 38+6 weeks’ gestation [8].
Responding to the NICE guidelines, a National Pregnancy in Diabetes (NPID) audit was established to document the pregnancy preparation, antenatal care and fetal health outcomes for pregnant women with type 1 and type 2 diabetes [9].
Here we present pregnancy outcomes of women with diabetes who delivered between 1 January 2015 and 31 December 2015. Our aims were to provide contemporary data on the rates of serious adverse pregnancy outcomes (congenital anomaly, stillbirth and neonatal death) and perinatal complications (preterm delivery, LGA and neonatal care admission), and to explore the relationship between maternal deprivation and clinic-to-clinic variations with maternal glycaemic control and folic acid supplementation. We also describe changes since the previous 2002/2003 CEMACH survey.
Methods
Healthcare professionals at each maternity unit completed standardised web-based data entry forms for every pregnant woman with diabetes who delivered between 1 January and 31 December 2015. As not all pregnancies resulted in a delivery these numbers included pregnancies ending in miscarriage or termination within this date range. All maternity units in England, Wales and the Isle of Man providing antenatal diabetes care were expected to participate (http://digital.nhs.uk/npid). Data were obtained only from women who provided written informed consent. The information leaflet and consent form met the Health Research Authority requirements for clinical audit, and research ethics approval was not required. Linkage with data collected in other systems (Hospital Episodes Statistics data, Patient Episode Database for Wales, National Diabetes Audit) allowed only a limited number of data items to be collected by local teams. This included information regarding type of diabetes, medications and folic acid use before conception. Data regarding pregnancy outcome was completed locally at 28 days after delivery, miscarriage or termination.
We defined pregestational diabetes as diabetes that had been diagnosed before pregnancy, and excluded women with diabetes who presented during pregnancy. Women with monogenic diabetes, or where there was doubt about whether they had type 1 or type 2 diabetes, or the type of diabetes data item was missing were classified as ‘other’ (these pregnancies were excluded from analyses comparing type 1 and type 2 diabetes). Glycaemic control was derived from HbA1c measurements, and the first and last recorded values during pregnancy were collected. HbA1c was measured locally using DCCT-aligned assays. We explored the relationship between maternal deprivation with glycaemic control and folic acid supplementation using an index of multiple deprivation score for women living in England and Wales where postcode details were recorded in the National Diabetes Audit [10]. For data protection of potentially sensitive information in the clinic-to-clinic comparisons, we included only clinics with at least ten completed pregnancy records; therefore, 130 clinics were included for type 1 diabetes and 103 clinics for type 2 diabetes comparisons.
We defined stillbirth as a fetal loss occurring after 24 weeks’ gestation, and neonatal death as death of a live born infant up to 28 days after delivery. We collected data on congenital anomalies for live births and terminations of pregnancy at any gestation, including for stillbirths and for fetal loss after 20 weeks’ gestation. The reported diagnoses for congenital anomaly were obtained from the hospital ICD-10 codes (www.who.int/classifications/icd/en/). We calculated the congenital anomaly rate as the number of infants with one or more congenital anomalies divided by the number of live births, terminations, stillbirths and fetal loss after 20 weeks’ gestation. Infant birthweight was adjusted for maternal ethnicity, height and weight, infant sex, and gestational age at delivery for singleton pregnancies using customised centiles with large and extreme LGA defined as >90th and >97.7th percentiles, respectively (GROW Centile Calculator v5.7.7.1, Gestation Network, www.gestation.net) [11].
Variables which were not normally distributed are given as median (interquartile range [IQR]), while normally distributed variables are given as mean (SD). Univariate analyses comparing the proportions between groups were performed using z tests and t tests for comparing continuous variables. We used Stata 8.0 for analyses and Poisson distribution to obtain 95% CIs for the rate and prevalence ratios.
Results
Participation
During the 12 month study period, 155 National Health Service (NHS) maternity clinics participated. Together they contributed 3044 pregnancies among 3036 women with diabetes, providing data for 3086 pregnancies (eight women had two pregnancies and 42 twin pregnancies were recorded). We report infant health outcomes for 2866 pregnancies that continued beyond 24 weeks’ gestation. Table 1 gives a description of the numbers of women and pregnancies according to type of diabetes.
Maternal characteristics
Almost half of the women included in the study (n = 1386; 46%) had type 2 diabetes, rising to more than 50% in large metropolitan regions (London, West Midlands, Yorkshire and Humber). Ninety per cent of Asian women and 71% of Black women had type 2 diabetes. As expected, women with type 2 diabetes were significantly older (33.6 vs 29.9 years; p < 0.001), had higher BMI (33.3 vs 26.8 kg/m2; p < 0.001), had shorter diabetes duration (4.8 vs 14.9 years; p < 0.001) and were more likely to live in the most deprived quintile of deprivation (38.5% vs 20.9%; p < 0.001) than women with type 1 diabetes (Table 2).
Prepregnancy preparation
Preconception folic acid
Women with type 2 diabetes were significantly less likely to take the recommended 5 mg dose of folic acid before conception compared with women with type 1 (22.5% vs 46.1%; p < 0.001; Table 2). There was also marked variation between clinics in the percentage of women with type 2 diabetes taking 5 mg folic acid (Fig. 1d); 33% of women attending the top quartile clinics took 5 mg folic acid compared with 15% in the lowest quartile (21.3% [15.4–33.2]). Over half the women with type 1 diabetes attending the top quartile clinics took 5 mg folic acid compared with less than a third in the lowest quartile clinics (42.9% [31.5–52.3]; Fig. 1b). Maternal deprivation was strongly associated with folic acid use among women with type 1 diabetes, with 75.1% use among women with type 1 diabetes living in the least deprived areas (vs 37.5% in the most deprived areas; p < 0.05, data not shown).
Variation between clinics in the percentage of women taking 5 mg folic acid and achieving target HbA1c levels <6.5% (48 mmol/mol) in early pregnancy. Percentage of women with type 1 diabetes: (a) achieving target HbA1c levels in early pregnancy and (b) taking 5 mg folic acid and at individual clinics. Percentage of women with type 2 diabetes: (c) achieving target HbA1c levels in early pregnancy and (d) taking 5 mg folic acid at individual clinics. The clinics are ranked from smallest number to greatest number of women achieving the targets left to right. Solid line, median; dashed lines, IQR
Glycaemic control in early pregnancy
Although glycaemic control was suboptimal in both type 1 and type 2 diabetes, women with type 2 diabetes were more than twice as likely to achieve target HbA1c levels of <6.5% (48 mmol/mol) in early pregnancy (38.3% vs 16.2%; p < 0.001; Table 2). Women achieving target HbA1c levels had lower BMI at booking (25.7 vs 27.0 kg/m2 for type 1, 31.9 vs 34.0 kg/m2 for type 2; p < 0.001). Women with type 1 diabetes who achieved target HbA1c levels were older (31.3 vs 29.8 years; p < 0.001) and lived in the least deprived areas, with almost one in four women in the least deprived areas achieving target HbA1c compared with one in ten women in the most deprived areas (24% vs 9.9%; p < 0.001). For women with type 2 diabetes, only maternal BMI (31.9 vs 34.0) and shorter diabetes duration (4.2 vs 5.4 years; both p < 0.001) were associated with achieving target HbA1c levels (data not shown). The percentage of women with type 1 and type 2 diabetes achieving target HbA1c levels in early pregnancy also varied greatly between clinics (14.3% [7.7–22.2] for type 1 and 37.0% [27.3–46.2] for type 2; Fig. 1a, c). The top quartile clinics had 22% of women with type 1 and 46% with type 2 diabetes achieving target HbA1c levels with 7% and 27%, respectively, in the lowest quartile clinics.
Presenting for antenatal care prior to 8 weeks’ gestation was more common in women with type 1 diabetes (54.4% vs 36.2%; p < 0.001; Table 2), again with substantial variation between clinics (55.0% [37.2–65.0] and 36.4% [21.7–50.0], respectively). Periconception exposure to potentially harmful medications, such as statins, ACE inhibitors or angiotensin receptor blockers, was less common in women with type 1 compared with type 2 diabetes (2.9% vs 8.6%; p < 0.001).
Glycaemic control in late pregnancy
As expected, maternal HbA1c levels decreased during pregnancy. After 24 weeks’ gestation in women with type 2 diabetes, 76.0% achieved target HbA1c levels <6.5% (48 mmol/mol) (Table 2) and 85.9% achieved HbA1c < 7.0% (53 mmol/mol) (Table 3). Only 40.0% and 59.5% of women with type 1 diabetes achieved these targets, respectively (p < 0.001).
Perinatal morbidity
Preterm delivery
While the majority of live singleton births were between 37+0 and 38+6 weeks (mean gestation 36.4 for type 1 and 37.1 for type 2; p < 0.001), the rates for preterm delivery before 37 weeks were 39.7% in women with type 1 and 21.7% in those with type 2 diabetes (p < 0.05; Table 2). Among women with suboptimal early glycaemic control (HbA1c level ≥ 6.5% [48 mmol/mol]) the preterm birth rate was significantly lower if they later achieved HbA1c levels <6.5% (48 mmol/mol) after 24 weeks’ gestation (30.4% vs 48.0% for type 1; 21.6% vs 35.7% for type 2, both p < 0.001; Fig. 2a).
LGA
The numbers of large and extreme LGA infants (birthweight >90th and >97.7th percentiles, respectively) were significantly higher for women with type 1 diabetes (46.4% and 29.4% for type 1 vs 23.9% and 14.0% for type 2, respectively; both p < 0.001; Table 2). As with preterm delivery, the LGA rates were significantly lower among women with suboptimal early glucose control if they later achieved HbA1c levels <6.5% (48 mmol/mol) (34.2% vs 54.9% for type 1; 19.0% vs 47.4% for type 2, both p < 0.001; Fig. 2b).
Neonatal intensive care unit admission
LGA infants were more likely to be admitted for neonatal care than infants appropriate for gestational age (32.1% vs 25.6% for type 1, 25.6% vs 11.4% for type 2; p < 0.05). Admission to neonatal care units was reduced among term infants (i.e. born at or after 37+0 weeks’ gestation) of women with suboptimal glycaemic control in early pregnancy if they later achieved HbA1c levels <6.5% (48 mmol/mol) (22.7% vs 33.4% for type 1 and 12.2% vs 23.6% for type 2; p < 0.05).
Comparisons with the 2002/2003 CEMACH data
Maternal and demographic characteristics
This cohort was larger than the previous CEMACH survey, with 685 more diabetes pregnancies and a striking increase in the proportion of pregnancies complicated by type 2 diabetes (Table 3). There was also more concentrated data focusing on pregnancy care across fewer clinics, with 3044 diabetes pregnancies across 155 maternity clinics (19.6 per clinic) in 2015, compared with 2359 diabetes pregnancies in 231 clinics (10.2 per clinic) in 2002/2003. The duration of diabetes was longer (by approximately 2 years) in both type 1 and type 2 diabetes. More women were taking folic acid supplementation before conception and more had a recorded first trimester measurement of HbA1c. There was no improvement in glucose control in type 1 diabetes but some improvement during late gestation in type 2 diabetes, with an increased proportion of women who achieved HbA1c < 7.0% (53 mmol/mol) after 24 weeks in 2015 (85.9% vs 75.4%; p < 0.05).
Serious adverse pregnancy outcomes
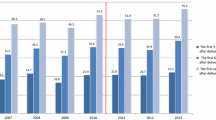
In 2015, the stillbirth rate was high (10.7/1000 for type 1 and 10.5/1000 for type 2; Table 3) compared with the general maternity population rate of 4.7/1000 [12]. However, it was almost 2.5-fold lower than in 2002/2003 (Fig. 3). The neonatal death rate was also high (8.1/1000 for type 1 and 11.4/1000 for type 2 diabetes), but unchanged compared with 2002/2003. The prevalence of congenital anomalies (including all major and minor anomalies detected at hospital discharge) was 46.2/1000 for type 1 and 34.6/1000 for type 2 diabetes (Table 3). These data are not directly comparable with the 2002/2003 data, which included only major congenital anomalies.
Stillbirth rate during the NPID audit 2015 compared with CEMACH 2002/2003 for women with type 1 and type 2 diabetes. Data presented are stillbirth rates per 1000 births with 95% CI. Dashed line, stillbirth rate for the general maternity population for 2015 (based on data from the Office for National Statistics [12])
Discussion
This large national study details the pregnancy outcomes of women with diabetes more than a decade after the 2002/2003 CEMACH survey. While the pregnancy outcomes of women with diabetes were still suboptimal compared with the general maternity population, substantial progress has been made with significant reductions in stillbirths in both type 1 and type 2 diabetes. There were fewer preterm deliveries, LGA infants and neonatal care unit admissions in women with type 2 compared with type 1 diabetes, reflecting the better antenatal glycaemic control in type 2 diabetes. Glucose control in women with type 1 diabetes was suboptimal, with persistently high rates of preterm delivery, LGA and neonatal care unit admissions. The highest rates of neonatal complications were seen in women with HbA1c levels ≥6.5% (48 mmol/mol) after 24 weeks’ gestation.
Over the past decade the proportion of pregnant women with type 2 diabetes has risen from 28% to 46% of all diabetes pregnancies, with type 2 now outnumbering type 1 diabetes pregnancies in some metropolitan areas. The proportion of women taking preconception folic acid supplementation has increased both in type 1 and type 2 diabetes, which is in contrast to some recent data suggesting a small decline (from 35% to 31%) in the general maternity population [13].
Our data demonstrate the ongoing healthcare inequalities between women with type 1 and type 2 diabetes and the striking contribution of maternal deprivation in type 1 diabetes. In women with type 1 diabetes, 75% of those living in the most socioeconomically advantaged areas took 5 mg preconception folic acid and 25% achieved target HbA1c levels in early pregnancy, whereas only 37% of women living in the most disadvantaged areas took folic acid and only 10% achieved target HbA1c levels in early pregnancy. This information highlights the need to more effectively target prepregnancy care to women living in deprived areas. Previous studies have shown that targeting all women of reproductive years can minimise the impact of maternal deprivation on prepregnancy care attendance, folic acid supplementation and early pregnancy glycaemic control [14].
It is disappointing that so few women with type 1 diabetes achieved the NICE recommended glycaemic control target for HbA1c in early and late pregnancy (16.1% and 40.0% respectively). We speculate that this is due to previously described physiological and pharmacological challenges of matching pre-meal insulin boluses to postprandial glucose profiles in early and late gestation [15, 16]. We have shown that while women achieving target glycaemic control are older, leaner and more socially advantaged, there is substantial variation across clinics, suggesting that the impact of clinic context is also important. Further work is needed to understand whether these clinic-to-clinic variations relate to clinic size and/or staff experience of implementing newer technologies such as insulin pump therapy and continuous glucose monitoring before and during pregnancy.
While there is much emphasis on improving preconception and first trimester glucose control to reduce congenital anomaly, stillbirth and neonatal death, our data also indicate the importance of optimal glucose control in late gestation for reducing the rates of preterm delivery, LGA infants and neonatal intensive care unit admission. An important take home message for women with unplanned pregnancy and/or suboptimal early glucose control is that achieving HbA1c < 6.5% (48 mmol/mol) after 24 weeks was very effective for reducing perinatal complications both in type 1 and type 2 diabetes.
The absolute risk of stillbirth has consistently remained 10–13/1000 over three diabetes pregnancy audit years, which now includes 6675 diabetes pregnancies [17]. Recent data from Sweden have comparable absolute stillbirth rates (15/1000) among women with type 1 diabetes [1]. However, the Swedish diabetes rates are still five times higher than the low background maternity population rates (3/1000) characteristic of high-income countries. In 2002/2003 there was a similar fivefold increase in stillbirths among women with diabetes in the UK [3].
The reductions in stillbirths in type 1 and type 2 diabetes are not solely due to improvements in the general maternity population [12], as the UK currently reports one of the slowest rates of decline in stillbirth of approximately 17% (from 5.3 to 4.4/1000 births) over the past decade [18]. Although there are clear maternal risk factors, including previous stillbirth, multiple pregnancy, nulliparity, diabetes, maternal age over 40 years, non-White ethnicity, smoking and obesity, most of the variability in stillbirth rates is independent of established risk factors [19, 20]. We can only speculate as to the possible explanations for recent improvements, which may include earlier elective birth recommendations (37+0 weeks’ gestation), tighter glycaemic control targets (HbA1c < 6.5% or 48 mmol/mol) and/or greater concentrations of women with diabetes among fewer maternity clinics.
Stillbirth is the most common cause of perinatal death [21], so it is surprising that the reduction in stillbirths was not accompanied by a reduction in the neonatal death rate (8.1 vs 9.6/1000 for type 1 and 11.4 vs 9.5/1000 for type 2) since 2002/2003. The reasons for this are unknown and will require further evaluation in larger datasets over longer time frames.
Our study is one of the largest to describe the pregnancy outcomes associated with contemporary diabetes care and includes over 3000 women with pregnancies complicated by diabetes. Our large sample size provides the statistical power for evaluating trends in serious but rare outcomes. Other large-scale studies conducted over 10–20 years in Sweden [1] and Finland [5] are less relevant to current clinical practice, and in particular to the increasing problem of type 2 diabetes in pregnancy [22]. Our cohort is larger than any previous studies of pregnant women with type 2 diabetes and confirms meta-analyses findings that there are no differences in the rates of congenital anomalies, stillbirths and perinatal deaths between type 1 and type 2 diabetes [23]. We do confirm important differences in the perinatal outcomes of type 1 and type 2 diabetes pregnancy with significantly lower rates of preterm delivery, LGA infants and neonatal intensive care unit admissions in type 2 diabetes.
Our study should be interpreted in the context of potential limitations. First, these are cross-sectional analyses, which preclude us from making causal inferences. Second, use of routinely collected data means we have little control over errors during data collection and variations due to differences in timing and laboratory methods for HbA1c levels. Third, because of the information governance requirements and the pre-specified nature of these analyses, we are unable to analyse whether there are significant, independent effects of HbA1c in early and late pregnancy and/or maternal BMI on neonatal outcomes. Furthermore, we cannot guarantee that data from all women and all maternity clinics are included, and we lack information for women who did not provide consent. The numbers of women who refuse consent is anecdotally very small. For 94 clinics that responded to an electronic survey, an average of one woman per clinic was unable to and/or refused consent (C. Cartwright, P. Curnow, C. Sylvester, B. Young, unpublished data). Having 3044 pregnancies in women providing consent is at least comparable to the 2359 pregnancies without consent in 2002/2003. We also cannot be certain that the 87 women where the type of diabetes is classified as ‘unknown’ did not have type 1 or type 2 diabetes.
More work is needed to ensure that women with type 2 diabetes and their community healthcare providers are aware of the importance of safe effective contraception and/or prepregnancy care. Further research is needed to better understand the impact of clinic size and whether centralisation in fewer, larger clinics would improve glucose control and pregnancy outcomes. It remains to be seen whether recent advances in continuous glucose monitoring and closed-loop insulin delivery will be effective for improving late gestation glucose control and reducing perinatal morbidity in type 1 diabetes pregnancy [24, 25]. For stillbirth, research to identify better predictors of placental dysfunction such as erythropoietin, pregnancy associated plasma protein A, alpha fetoprotein and angiogenic/antiangiogenic factors in women with diabetes is needed [26,27,28].
The NPID data provides information that can be used at the level of individual maternity clinics so service users, healthcare professionals and funders can make informed healthcare choices. It has demonstrated substantial nationwide progress in diabetes stillbirth reductions but highlights ongoing challenges to consistently improve glucose control and reduce perinatal complications in type 1 diabetes pregnancy.
Abbreviations
- CEMACH:
-
Confidential Enquiry into Maternal and Child Health
- GROW:
-
Gestation-related optimal weight
- IQR:
-
Interquartile range
- LGA:
-
Large for gestational age
- NHS:
-
National Health Service
- NPID:
-
National Pregnancy in Diabetes
- NICE:
-
National Institute for Health and Care Excellence
References
Persson M, Norman M, Hanson U (2009) Obstetric and perinatal outcomes in type 1 diabetic pregnancies: a large, population-based study. Diabetes Care 32:2005–2009
Evers IM, de Valk HW, Visser GH (2004) Risk of complications of pregnancy in women with type 1 diabetes: nationwide prospective study in the Netherlands. BMJ 328:915
Macintosh MC, Fleming KM, Bailey JA et al (2006) Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ 333:177
Evers IM, de Valk HW, Mol BW, ter Braak EW, Visser GH (2002) Macrosomia despite good glycaemic control in type I diabetic pregnancy; results of a nationwide study in the Netherlands. Diabetologia 45:1484–1489
Klemetti M, Nuutila M, Tikkanen M, Kari MA, Hiilesmaa V, Teramo K (2012) Trends in maternal BMI, glycaemic control and perinatal outcome among type 1 diabetic pregnant women in 1989-2008. Diabetologia 55:2327–2334
Confidential Enquiry into Maternal and Child Health (2005) Pregnancy in women with type 1 and type 2 diabetes in 2002-03, England, Wales and Northern Ireland. CEMACH, London
NICE guideline 63 (2008) Diabetes in pregnancy. Management of diabetes and its complications from the pre-conception to the postnatal period. Available from www.nice.org. Accessed 26 Nov 2016
NICE guideline 63 (2015) Diabetes in pregnancy. Management of diabetes and its complications in pregnancy from the pre-conception to the postnatal period. Available from https://www.niceorguk/guidance/ng3. Accessed 26 Nov 2016
Murphy HR, Bell R, Holt RI et al (2013) The National Pregnancy in Diabetes Audit: measuring the quality of diabetes pregnancy care. Diabet Med 30:1014–1016
Office of the Deputy Prime Minister (2004) The English indices of deprivation 2004 (revised). Office of the Deputy Prime Minister, London
Gardosi J, Francis A 2015. Customised weight centile calculator. GROW v6.7.7.1. Available from http://www.gestation.net/birthweight_centiles/centile_object.htm. Accessed 26 Nov 2016
Office for National Statistics (2015) Births in England and Wales. Available from http://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2015. Accessed 26 Nov 2016
Bestwick JP, Huttly WJ, Morris JK, Wald NJ (2014) Prevention of neural tube defects: a cross-sectional study of the uptake of folic acid supplementation in nearly half a million women. PLoS One 9:e89354
Murphy HR, Roland JM, Skinner TC et al (2010) Effectiveness of a regional prepregnancy care program in women with type 1 and type 2 diabetes: benefits beyond glycemic control. Diabetes Care 33:2514–2520
Murphy HR, Elleri D, Allen JM et al (2012) Pathophysiology of postprandial hyperglycaemia in women with type 1 diabetes during pregnancy. Diabetologia 55:282–293
Goudie RJ, Lunn D, Hovorka R, Murphy HR (2014) Pharmacokinetics of insulin aspart in pregnant women with type 1 diabetes: every day is different. Diabetes Care 37:e121–e122
Holman N, Bell R, Murphy H, Maresh M (2014) Women with pre-gestational diabetes have a higher risk of stillbirth at all gestations after 32 weeks. Diabet Med 31:1129–1132
Flenady V, Wojcieszek AM, Middleton P et al (2016) Stillbirths: recall to action in high-income countries. Lancet 387:691–702
Stillbirth Collaborative Research Network Writing Group (2011) Association between stillbirth and risk factors known at pregnancy confirmation. JAMA 306:2469–2479
Familiari A, Scala C, Morlando M, Bhide A, Khalil A, Thilaganathan B (2016) Mid-pregnancy fetal growth, uteroplacental doppler indices and maternal demographic characteristics: role in prediction of stillbirth. Acta Obstet Gynecol Scand 95:1313–1318
Smith GC (2016) Screening and prevention of stillbirth. Best Pract Res Clin Obstet Gynaecol 10:1–12
Temple R, Murphy H (2010) Type 2 diabetes in pregnancy: an increasing problem. Best Pract Res 24:591–603
Balsells M, Garcia-Patterson A, Gich I, Corcoy R (2009) Maternal and fetal outcome in women with type 2 versus type 1 diabetes mellitus: a systematic review and metaanalysis. J Clin Endocrinol Metab 94:4284–4291
Feig DS, Asztalos E, Corcoy R et al (2016) CONCEPTT: continuous glucose monitoring in women with type 1 diabetes in pregnancy trial: a multi-center, multi-national, randomized controlled trial—study protocol. BMC Pregnancy Childbirth 16:167
Stewart ZA, Wilinska ME, Hartnell S et al (2016) Closed-loop insulin delivery during pregnancy in women with type 1 diabetes. N Engl J Med 375:644–654
Teramo K, Kari MA, Eronen M, Markkanen H, Hiilesmaa V (2004) High amniotic fluid erythropoietin levels are associated with an increased frequency of fetal and neonatal morbidity in type 1 diabetic pregnancies. Diabetologia 47:1695–1703
Conde-Agudelo A, Bird S, Kennedy SH, Villar J, Papageorghiou AT (2015) First- and second-trimester tests to predict stillbirth in unselected pregnant women: a systematic review and meta-analysis. BJOG 122:41–55
Chaiworapongsa T, Romero R, Korzeniewski SJ et al (2013) Maternal plasma concentrations of angiogenic/antiangiogenic factors in the third trimester of pregnancy to identify the patient at risk for stillbirth at or near term and severe late preeclampsia. Am J Obstet Gynecol 208(287):e1–e15
Acknowledgements
The authors are extremely grateful to all of the women who consented to participate and to local antenatal diabetes healthcare teams for their support with data entry. We are also grateful to L. Fargher (Diabetes UK, London, UK) for her NPID engagement activities and to P. Knighton from NHS Digital (NHS Digital, Leeds, UK), formerly known as the Health and Social Care Information Centre, for statistical input. Parts of these data were presented at the NPID meeting, London, 10 November 2016. The full NPID audit report 2015 was published online 21 October 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data availability
Further details of the data collection methodology, individual clinic data and the full audit reports for healthcare professionals and service users are available from http://content.digital.nhs.uk/npid.
Funding
The NPID audit is commissioned by the Healthcare Quality Improvement Partnership as part of the National Clinical Audit programme funded by NHS England and the Welsh government. The 2015 audit was prepared in collaboration with NHS Digital and supported by Diabetes UK and Public Health England.
Duality of interest
HRM sits on a scientific advisory board for Medtronic (insulin pump manufacturer). The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
HRM, RB, MMa, MMo, NLB, BY made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. CC, PC and CS analysed the data. HRM drafted the manuscript. All authors critically reviewed the manuscript for important intellectual content and gave final approval for publication. HRM is the guarantor of this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Murphy, H.R., Bell, R., Cartwright, C. et al. Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: a prospective nationwide study. Diabetologia 60, 1668–1677 (2017). https://doi.org/10.1007/s00125-017-4314-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-017-4314-3