Abstract
Aims/hypothesis
Chronic exposure to high concentrations of glucose has consistently been demonstrated to impair endothelium-dependent, nitric oxide (NO)-mediated vasodilation. In contrast, several clinical investigations have reported that acute exposure to high glucose, alone or in combination with insulin, triggers vasodilation. The aim of this study was to examine whether elevated glucose itself stimulates endothelial NO formation or enhances insulin-mediated endothelial NO release.
Methods
We measured NO release and vessel tone ex vivo in porcine coronary conduit arteries (PCAs). Intracellular Ca2+ was monitored in porcine aortic endothelial cells (PAECs) by fura-2 fluorescence. Expression of the Na+/glucose cotransporter-1 (SGLT-1) was assayed in PAECs and PCA endothelium by RT-PCR.
Results
Stimulation of PCAs with d-glucose, but not the osmotic control l-glucose, induced a transient increase in NO release (EC50≈10 mmol/l), mediated by a rise in intracellular Ca2+ levels due to an influx from the extracellular space. This effect was abolished by inhibitors of the plasmalemmal Na+/Ca2+ exchanger (dichlorobenzamil) and the SGLT-1 (phlorizin), which was found to be expressed in aortic and coronary endothelium. Alone, d-glucose did not relax PCA, but did augment the effect of insulin on NO release and vasodilation.
Conclusions/interpretation
An increased supply of extracellular d-glucose appears to enhance the activity of the endothelial isoform of nitric oxide synthase by increasing intracellular Na+ concentrations via SGLT-1, which in turn stimulates an extracellular Ca2+ influx through the Na+/Ca2+ exchanger. This mechanism may be responsible for glucose-enhanced, insulin-dependent increases in tissue perfusion (including coronary blood-flow), thus accelerating glucose extraction from the blood circulation to limit the adverse vascular effects of prolonged hyperglycaemia.
Similar content being viewed by others
Introduction
Chronic exposure to high glucose has been consistently demonstrated to adversely affect endothelial function and impair nitric oxide (NO)-dependent vasodilation, and has been implicated in diabetes-associated cardiovascular morbidity and mortality [1, 2, 3, 4]. Although insulin resistance and glucose intolerance are important risk factors for type 2 diabetes, the majority of subjects who exhibit these alterations do not develop diabetes or persistent endothelial dysfunction [5, 6]. Thus, adaptive responses, particularly maintenance of vascular function, may prevent manifestation of diabetic symptoms. Hyperinsulinaemia and post-prandial hyperglycaemia are the main features of the ‘pre-diabetic’ state [7, 8]. While the vasodilating effects of insulin are established [9, 10], the direct vascular actions of short-term hyperglycaemia are largely unknown. Studies investigating the effects of high glucose on macrovascular and microvascular perfusion have yielded conflicting results: some have shown attenuated vasodilation [11, 12, 13, 14, 15, 16], some have demonstrated enhanced vasodilation [17, 18, 19, 20], whereas others found no changes in vascular tone [21, 22, 23]. The present study was designed to gain deeper insights into the immediate effects of high glucose on endothelial NO formation and vascular tone, and its stimulatory role on the vascular effects of insulin.
Materials and methods
Chemicals
Porcine insulin was obtained from Berlin-Chemie (Insulin S, 40 IU/ml; Berlin, Germany). Inorganic salts and solvents were from VWR International (Darmstadt, Germany). Unless otherwise noted, all other reagents were purchased from Sigma-Aldrich (Deisenhofen, Germany).
Real-time measurement of nitric oxide levels
Measurements were performed ex vivo using porcine coronary conduit arteries (PCAs), which were freshly dissected at the local abattoir (Fleischversorgung Köln e.V., Cologne, Germany) from the hearts of domestic pigs aged 7–9 months. Luminal NO release was monitored amperometrically in real time by a NO-selective microsensor (ISO-NO-Meter, WPI, Sarasota, Fla., USA) as described previously [24]. Briefly, PCA segments (approximately 2 cm in length) were opened longitudinally and mounted in organ baths containing 10 ml HEPES-modified Krebs buffer (140.0 mmol/l NaCl, 5.0 mmol/l KCl, 2.0 mmol/l CaCl2, 1.0 mmol/l mgCl2, 10.0 mmol/l HEPES and 5.0 mmol/l d-glucose, adjusted to pH 7.40) at 25 °C. The sensor was positioned under microscopic control at a distance of 200–300 µm above the endothelial surface. All experiments were performed in a non-cumulative fashion by using separate vessels for each concentration of test compound.
Measurement of vascular tone
The vascular tone of the PCAs was monitored isometrically as described previously [24]. Briefly, PCA rings (length 3–4 mm) were mounted in carbogen-aerated organ chambers containing 10 ml Tyrode solution (161.1 mmol/l Na+, 5.4 mmol/l K+, 1.8 mmol/l Ca2+, 1.1 mmol/l mg2+, 148.0 mmol/l Cl–, 23.8 mmol/l HCO3 –, 0.4 mmol/l H2PO4 – and 5.0 mmol/l d-glucose) at 37 °C. Single concentrations of test compounds (50 µl) were applied to vessels pre-contracted with PGF2α (25 µmol/l). Vasodilator responses are expressed as a percentage of the PGF2α pre-contraction.
Measurement of intracellular Ca2+ levels
Culture of porcine aortic endothelial cells
Porcine aortic endothelial cells (PAECs) were enzymatically (dispase, 1 mg/ml; Boehringer Mannheim, Mannheim, Germany) isolated from segments of porcine thoracic aorta and cultured in M199 (Gibco-Invitrogen, Karlsruhe, Germany) supplemented with 10% (v/v) FCS (Gibco-Invitrogen), 100 mg/l penicillin G, 100 mg/l streptomycin, 2 mmol/l l-glutamine and 15 mmol/l HEPES, as described previously [25]. Experiments were performed with confluent cells in passage 2 seeded on glass coverslips.
Ratiometric imaging of fura-2 fluorescence
This method has been described previously [25, 26]. Briefly, PAEC monolayers on coverslips were loaded in M199 with the cell-permeable fluorescent dye fura-2-acetomethoxyester (1 µmol/l) for 30 min at 37 °C; de-esterification of fura-2-acetomethoxyester to non-permeable fura-2 was completed in fresh M199 by a further 15 min incubation at 37 °C. Fluorescence signals of intracellular fura-2–Ca2+ complexes were recorded at 25 °C on an inverted epifluorescence microscope (Diaphot TMD; Nikon, Tokyo, Japan) using a ×40 objective lens (Fluor 40; Nikon). The excitation wavelength alternated every 0.5 s between 340 and 380 nm; emission was monitored at 510 nm. Intracellular Ca2+ was calculated from the 340/380 nm ratios of fluorescence intensities using the equation of Grynkiewicz et al. [26]. The traces represent the average intracellular Ca2+ concentration of 6 to 12 cells in the same microscopic field.
Measurement of superoxide generation
Superoxide generation was measured in immortalised HUVECs (EA.hy 926) [27] by lucigenin-enhanced chemiluminescence. The cells were grown to confluence on glass coverslips and then incubated for the times indicated with either high d-glucose or l-glucose (osmotic control) at 37 °C. After addition of 2.5 µmol/l lucigenin, cumulative luminescence intensity was recorded for 60 s using the FB-12 Sirius Single-Probe Luminometer (Berthold detection systems, Pforzheim, Germany). The immortalised HUVECs (EA.hy 926) show morphologic and functional similarities to the primary PAECs; however, these primary cultures tend to de-differentiate, resulting in lower and less consistent signal intensities than the immortalised cultures. Hence, to obtain more reliable results, we used the EA.hy 926 cell line instead of the PAECs for monitoring the time course of glucose-induced superoxide formation.
Reverse transcription and PCR of Na+/glucose cotransporter-1 mRNA
Total RNA was isolated from cloned porcine proximal tubule kidney cells (LLC-PK1), from PAECs in passage 2, and from the mechanically removed endothelial layer of freshly dissected PCA by guanidinium thiocyanate / phenol chloroform extraction [28]. The RNA was reversed-transcribed to cDNA using the Superscript First-Strand Synthesis System (Invitrogen, Karlsruhe, Germany). Aliquots of cDNA were amplified with primers specific for the Na+/glucose cotransporter-1 (SGLT-1) and the housekeeping gene β-actin. To confirm identity, amplification products (SGLT-1 DNA bands) were sequenced in both directions by Taq dideoxy terminator cycle sequencing (ABI Prism BigDye Terminator v2.0 Cycle Sequencing Kit; Applied Biosystems, Foster City, Calif., USA).
Data analysis
Extrapolated Emax and EC50 values of NO and tone measurements were derived from sigmoid regression curves of the concentration–response data and are expressed as arithmetic means ± 95% CI. Other values are expressed as means ± SEM. Differences between means were assessed by the two-tailed t test or ANOVA for multiple comparisons. A p value of less than 0.05 was considered statistically significant.
Results
Acute effects of glucose on vascular nitric oxide formation
Acute stimulation of PCAs with d-glucose increased endothelial NO release in a concentration-dependent manner, producing an Emax of 4.5±0.2 nmol/l NO at an EC50 of 10.7±1.0 mmol/l d-glucose (n=6). The osmotic control (l-glucose) did not significantly elevate NO levels (Fig. 1a). The maximum NO elevation achieved after stimulation with a single dose of 20 mmol/l d-glucose was 4.0±0.6 nmol/l; the NO signal occurred after a delay of 0.9±0.2 min and showed a monophasic time course consisting of a plateau that lasted for 4.5±0.4 min (n=6) (Fig. 1b). In endothelium-denuded PCAs, d-glucose did not induce NO release, thus identifying the endothelial layer as the only source of NO. The NO-releasing effects of high d-glucose were blunted in the presence of the non-selective nitric oxide synthase inhibitor l-N G-monomethyl arginine (l-NMMA, 100 µmol/l; Emax=1.6±0.3 nmol/l, n=6). Conversely, the response was not diminished in the presence of 1400 W, a specific inhibitor of the inducible and neuronal isoforms of nitric oxide synthase (5 µmol/l; Emax=4.4±0.4 nmol/l, n=6). This finding suggests that the d-glucose-mediated increase in NO was entirely due to stimulation of the endothelial isoform of nitric oxide synthase (eNOS).
Concentration–response curves of sugar-induced plateau NO release from PCAs after pre-incubation for 30–45 min in normal glucose buffer (5 mmol/l d-glucose). a. The NO release induced by d-galactose (black squares), l-glucose (black upward triangles), d-glucose (black circles), and d-glucose after NO synthase inhibition with 100 µmol/l l-NMMA (white circles) in PCAs, and d-glucose in endothelium-denuded arteries (black downward triangles). b. Original trace of the NO stimulation induced by 20 mmol/l d-glucose. c. The NO release induced by 20 mmol/l d-glucose after pre-incubation with increasing concentrations of the NCX blocker dichlorobenzamil. d. The NO release induced by 20 mmol/l d-glucose after pre-incubation with increasing concentrations of the SGLT blocker phlorizin. The data points show the arithmetic means ± SEM of 5 to 6 independent experiments each. * p<0.05; ** p<0.01; *** p<0.001 vs stimulation with 20 mmol/l d-glucose alone by two-tailed t test
Involvement of Ca2+ in glucose-induced nitric oxide formation
It is well established that eNOS is activated by an increase in intracellular Ca2+. Since the NO response to high d-glucose was depressed in the presence of a low extracellular concentration of Ca2+ and in the presence of Ni2+ (an inhibitor of divalent cation entry) (Table 1), stimulation of eNOS by d-glucose is likely to involve an influx of extracellular Ca2+. We therefore investigated whether Ca2+-dependent eNOS stimulation is mediated by activation of endothelial receptor-operated Ca2+ channnels. However, neither inhibition of capacitative Ca2+ entry by SK&F 96365, nor inhibition of the cAMP-dependent opening of plasmalemmal Ca2+ channels by the adenylate cyclase blocker 2′,5′-dideoxyadenosine-3′-diphosphate (ddAdoPP), diminished the NO response to d-glucose (Table 1).
Acute effects of glucose on intracellular Ca2+
The crucial role of Ca2+ in the NO response to d-glucose was supported by direct measurement of total intracellular Ca2+ concentrations in PAECs using fura-2 fluorescence. Supplementation of normal glucose buffer (5 mmol/l d-glucose) with an additional 20 mmol/l d-glucose caused a small transient increase in intracellular Ca2+. The osmolar control (20 mmol/l l-glucose) did not change resting intracellular Ca2+ levels (Fig. 2a, Table 2). The d-glucose-mediated rise in intracellular Ca2+ was lost after the abolition of the transmembrane Ca2+ gradient and in the presence of Ni2+ (Table 2).
Original traces of free intracellular calcium in PAECs. a. The increase in intracellular Ca2+ after stimulation with 20 mmol/l l-glucose (dotted line, bottom), d-glucose (solid line, middle), and d-glucose following pre-treatment for 30 min with 1 µmol/l cytochalasin B (dashed graph, top). b. The increase in intracellular Ca2+ induced by 10 µmol/l of the sodium ionophore monensin. c. The increase in intracellular Ca2+ after stimulation of PAECs with 20 mmol/l d-glucose after pre-treatment with 30 µmol/l dichlorobenzamil. d. The increase in intracellular Ca2+ after stimulation of PAECs with 20 mmol/l d-glucose after pre-treatment with 100 µmol/l phlorizin
Involvement of Ca2+ transporters in glucose-mediated eNOS activation
Cytoplasmic calcium homeostasis is largely regulated by the plasma membrane Ca2+ ATPase (PMCA), the endoplasmic Ca2+ ATPase (SERCA), and the plasmalemmal Na+/Ca2+ exchanger (NCX) [29]. Inhibition of PMCA with La3+, or SERCA with thapsigargin (for ≥30 min following the initial NO stimulation produced by delayed cytoplasmic Ca2+ removal) did not affect the d-glucose-induced endothelial NO response. This suggests that the Ca2+-dependent activation of eNOS by d-glucose does not involve the inhibition of cytoplasmic Ca2+ clearance by the outward rectifying Ca2+ pumps or the refilling of internal Ca2+ stores (Table 1). However, the NCX inhibitor dichlorobenzamil prevented the d-glucose-induced NO release in a concentration-dependent manner (Fig. 1c). The NCX is driven by the plasmalemmal Na+ gradient. Thus, on removal of the transmembrane Na+ gradient by the substitution of normal Na+ buffer (140 mmol/l Na+) with a low Na+ solution (20 mmol/l Na+ plus 120 mmol/l choline chloride as osmotic substitute), d-glucose-induced NO elevations were lost (Table 1). Similarly, when PCAs previously incubated in normal glucose and sodium buffer were treated with the Na+ ionophore monensin (10 µmol/l), increasing the intracellular Na+ concentration, the extent and duration of NO release was similar to that observed with high d-glucose (5.3±0.2 nmol/l NO and 5.2±0.4 min respectively, n=6). Co-incubation of monensin (10 µmol/l) with dichlorobenzamil (30 µmol/l) reduced the maximal NO signal to 1.8±0.2 nmol/l NO (p<0.001, n=5). Modulation of NO was accompanied by corresponding effects on intracellular Ca2+. In PAECs, the d-glucose-induced increase in intracellular Ca2+ was completely blocked by the presence of dichlorobenzamil (Fig. 2c), while stimulation with monensin elicited a transient plateau-like increase in intracellular Ca2+ (Fig. 2b).
Coupling of high glucose with NCX-dependent eNOS activation
The NO response to 20 mmol/l d-glucose (but not to l-glucose) was enhanced after blocking GLUT1 with cytochalasin B, the plateau NO increase and duration of the plateau being about 40% higher than the corresponding values in the absence of cytochalasin B (Table 1). The cytochalasin B-enhanced NO response was strongly related to a greater and longer-lasting intracellular Ca2+ response (Fig. 2a, Table 2). In contrast, specific competitive inhibition of SGLTs with phlorizin suppressed the d-glucose-induced NO response in a concentration-dependent manner (Fig. 1d), and abolished the increase in intracellular calcium (Fig. 2d). The transporter isoforms SGLT-1 and GLUT1 have been shown to transport d-galactose as efficiently as d-glucose [30, 31]. Accordingly, the effect of d-galactose on endothelial NO release (Emax=4.1±0.4 nmol/l, 4.2±0.3 min, n=5) (Fig. 1a, Table 1) and intracellular Ca2+ (Table 2) was similar to that observed with d-glucose. Both of these responses were blocked in the presence of phlorizin, and were enhanced by cytochalasin B (Tables 1 and 2).
PCR analysis
Amplification and sequencing of cDNA obtained from porcine coronary and aortic endothelial cells with SGLT-1-specific primers confirmed the presence of SGLT-1 mRNA in vascular endothelium, with cDNA from LLC-PK1 cells serving as a positive control [32] (Fig. 3).
PCR of cDNA derived from the total RNA of different porcine cell types. Lane 1, β-actin (363 bp); Lane 2, β-actin (negative control, i.e. RT-PCR without the reverse transcriptase); Lane 3, SGLT-1 (308 bp); Lane 4, SGLT-1 (negative control); and Lane 5, DNA ladder (100–1500 bp). The following oligonucleotide primers were used: SGLT-1 (sense) 5′-CTG GAT CCA GAG GAG GAG GAC AT-3′; SGLT-1 (antisense) 5′-GCC TGC AGG GCA CAG CCT GTG-3′ [49]; β-actin (sense) 5′-TCC CTG GAG AAG AGC TAC GA-3′; and β-actin (antisense) 5′-ACA TCT GCT GGA AGG TGG AC-3′
Acute effects of glucose on vascular tone
Although d-glucose induced NO release, in myographic experiments, stimulation of PCA rings incubated in normal glucose buffer (5 mmol/l glucose) with additional d-glucose (up to 50 mmol/l) did not alter vascular tone (Fig. 4a). The hyperosmotic control, l-glucose, and d-galactose also failed to cause significant relaxation or contraction. Similarly, stimulation of endothelium-denuded PCA rings with high d-glucose did not affect vascular tone (data not shown). However, following pre-incubation of vessels with cytochalasin B, the addition of 20 mmol/l d-glucose or d-galactose to endothelium-intact PCAs induced marked relaxation (Fig. 4a).
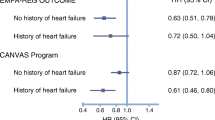
Relaxation of PCAs. a. Concentration–response curves of relaxation induced by d-glucose after pre-incubation of PCAs in normal glucose buffer (5 mmol/l d-glucose) for 30 min in the absence (black circles) and presence of 1 µmol/l cytochalasin B (black squares). b. Amplification of insulin-induced relaxation (5 IU/l insulin, dashed line) by co-incubation with increasing concentrations of d-glucose. c. Concentration–response curves of relaxation induced by: insulin alone (black upward triangles); co-stimulation with insulin plus 20 mmol/l d-glucose (black squares) or l-glucose (white downward triangles); insulin after 30 min pre-incubation with 100 µmol/l l-NMMA (black circles), 25 µmol/l genistein (white squares) or 1 µmol/l wortmannin (black downward triangles); and by insulin in endothelium-denuded arteries (white circles). d. Effect of pre-incubation time in high glucose buffer (25 mmol/l d-glucose) on relaxation in response to 5 IU/l insulin alone (black circles) or to 5 IU/l insulin plus 20 mmol/l d-glucose (white circles) compared with the effect of pre-incubation in high glucose buffer followed by 60 min incubation in normal glucose buffer on relaxation in response to 5 IU/l insulin (white upward triangles) or to 5 IU/l insulin plus 20 mmol/l d-glucose (black squares). Data points show the arithmetic means ± SEM of 4–6 independent experiments. * p<0.05; ** p<0.01; *** p<0.001 vs control by two-tailed t test
Involvement of glucose-facilitated arginine transport in nitric oxide formation and relaxation
Additionally, we investigated whether d-glucose amplified the stimulatory effect of the eNOS substrate l-arginine on NO release and vasodilation. The addition of 20 mmol/l d-glucose moderately (in a sub-additive manner) enhanced NO formation and relaxation in response to l-arginine. However, this effect attained significance only at l-arginine concentrations of ≥0.3 mmol/l and was absent when l-arginine was co-incubated with 20 mmol/l l-glucose (Fig. 5).
Glucose-mediated amplification of l-arginine-induced NO release (a) and relaxation (b) PCAs. PCA segments were incubated in normal d-glucose buffer (5 mmol/l) for 1 h prior to stimulation with l-arginine (black circles), l-arginine plus 20 mmol/l d-glucose (black squares), or l-arginine + 20 mmol/l l-glucose (white circles). Data points show the arithmetic means ± SEM of 4 or 5 independent experiments. * p<0.05; ** p<0.01 vs l-arginine alone by two-tailed t test
Additive effects of d-glucose and insulin on nitric oxide formation and vasorelaxation
Stimulation of PCAs with insulin in normal glucose buffer (5 mmol/l glucose) increased endothelial NO formation in a concentration-dependent manner, producing an Emax of 7.9±0.8 nmol/l NO at an EC50 of 24.3±4.5 mU/l insulin (Fig. 6a). This effect was abolished in the presence of the receptor/tyrosine kinase (RTK) blocker genistein and the phosphatidylinositol 3′-OH kinase (PI3 K) blocker wortmannin (Fig. 6b), but remained unchanged in the presence of Ni2+, phlorizin and dichlorobenzamil (Table 3). Compared with insulin alone, simultaneous stimulation of PCAs with insulin and increasing concentrations of d-glucose (but not l-glucose) amplified the endothelial NO response in a concentration-dependent and additive fashion (Fig. 6a,c). Co-stimulation with d-galactose and insulin evoked a similar potentiation of the NO signal (Fig. 6b, Table 3). Pre-treatment of PCAs with genistein or wortmannin reduced the NO response to combinations of insulin and high glucose to levels observed on insulin stimulation alone (Fig. 6b), whereas pre-treatment with phlorizin reduced the response to levels seen on high glucose stimulation alone (Table 3). Together, wortmannin and phlorizin almost completely suppressed the high d-glucose/insulin-induced NO elevation, producing results similar to those obtained when endothelium-denuded PCAs were employed (Fig. 6a). The combination of high d-glucose/insulin plus cytochalasin B provoked a further amplification of the NO signal, while cytochalasin B did not amplify the NO response to insulin in normal glucose buffer (Table 3).
Effects of glucose on insulin-induced NO release from PCAs. a. Concentration–response curves of NO release stimulated by: different concentrations of insulin alone (black downward triangles); by insulin plus 20 mmol/l d-glucose (black squares) or l-glucose (white upward triangles); insulin plus 20 mmol/l d-glucose after 30 min pre-incubation with 1 µmol/l wortmannin and 100 µmol/l phlorizin (white diamonds); and insulin plus 20 mmol/l d-glucose in endothelium-denuded arteries (black diamonds). b. The NO release induced by: co-stimulation of insulin with 20 mmol/l d-galactose (black squares); insulin alone after 30 min pre-incubation of PCAs with 25 µmol/l genistein (white circles) or 1 µmol/l wortmannin (black circles); and insulin plus 20 mmol/l d-glucose after 30 min pre-incubation of PCAs with 25 µmol/l genistein (white downward triangles) or 1 µmol/l wortmannin (black upward triangles). The dashed line indicates the mean NO stimulation by 20 mmol/l d-glucose. c. Amplification of insulin-induced NO release (0.5 IU/l insulin, dashed line) by co-incubation with increasing concentrations of d-glucose. d. Effect of pre-incubation time in high glucose buffer (25 mmol/l d-glucose) on NO release induced by 0.5 IU/l insulin alone (white circles), 20 mmol/l d-glucose alone (black squares), and by co-stimulation with 0.5 IU/l insulin plus 20 mmol/l d-glucose (black circles). e. Effect of pre-incubation of PCAs in high glucose buffer followed by 60 min incubation in normal glucose buffer (5 mmol/l d-glucose) on NO release induced by 0.5 IU/l insulin alone (white circles), 20 mmol/l d-glucose alone (black squares), and by co-stimulation with 0.5 IU/l insulin plus 20 mmol/l d-glucose (black circles). Data points show the arithmetic means ± SEM of 5 or 6 independent experiments. * p<0.05; ** p<0.01; *** p<0.vs stimulation with 0.5 IU/l insulin alone by two-tailed t test
Treatment of PCA rings with insulin plus high d-glucose (but not l-glucose) amplified insulin-dependent relaxation in a concentration-dependent manner (Fig. 4b). Relaxation was further increased by pre-incubation with cytochalasin B (Table 4), and was blunted by l-NMMA, genistein and wortmannin. Endothelium-denuded vessels completely failed to relax in response to insulin plus high d-glucose (Fig. 4c). There were no differences in the extent of inhibition in the presence or absence of high d-glucose (Table 4). Pre-treatment of PCAs with Ni2+, dichlorobenzamil or phlorizin reduced relaxation to levels observed with insulin stimulation alone (Table 4). Co-incubation with insulin and d-galactose mimicked the potentiating effects of d-glucose (Table 4).
Nitric oxide response and vasorelaxation after prolonged glucose overload
Prolonged exposure of coronary rings to high d-glucose caused a progressive loss of the acute stimulatory effects of both d-glucose and insulin on NO synthesis. After only 2 h of incubation with 25 mmol/l d-glucose, the potentiation of insulin-mediated NO release by high d-glucose was absent (Fig. 6d). The observed effects on NO release were in accordance with myographic experiments. Prolonged treatment with 25 mmol/l d-glucose attenuated relaxation in response to insulin and abolished the potentiating effect of high d-glucose on insulin-mediated relaxation (Fig. 4d). The NO and vascular responses of the PCAs to combinations of insulin plus d-glucose were only partially restored by incubation for 1 h in normal glucose buffer (Figs. 4d, 6e).
An increase in endothelial cell superoxide formation was observed after 24 h of incubation with high d-glucose, but not after 2 h of incubation (Fig. 7); thus, we were able to rule out the possibility that NO bioavailability and consequent vasodilation were reduced by glucose-enhanced superoxide generation. In keeping with this finding, in PCAs incubated in 25 mmol d-glucose for 2 h, the NO and vascular responses to d-glucose or insulin could not be restored by co-incubation with the superoxide scavangers vitamin C (2 mmol/l), trolox (2 mmol/l), superoxide dismutase (copper/zinc superoxide dismutase from bovine erythrocytes, 10 µmol/l) or the cell-permeable SOD analogue Mn(III) tetra(4-benzoic acid)porphyrin chloride (10 µmol/l) (data not shown).
Superoxide generation in EA.hy 926 cells after 2 h and 24 h of incubation in normal glucose buffer (5 mmol/l d-glucose, black bars), 20 mmol/l d-glucose (light grey bars), and in 20 mmol/l l-glucose (dark grey bars). Chemiluminescence intensities are given relative to the normal glucose buffer (NGB) control. Values shown represent the arithmetic means ± SEM of at least 8 experiments. * p<0.001 vs the normal glucose buffer control by two-tailed t test with Holm correction
Intracellular Ca2+ response after prolonged glucose overload
Stimulation of PAECs in normal glucose buffer with insulin (5 IU/l) did not alter intracellular Ca2+ concentrations (data not shown), while the response to insulin/high d-glucose was similar to that observed with to d-glucose alone (Table 2). Following incubation of the PAECs with 25 mmol/l d-glucose for 2 h, stimulation with additional d-glucose did not elicit an increase in intracellular Ca2+. However, treatment of the glucose-loaded PAECs with normal glucose buffer for 1 h restored the stimulatory effect of d-glucose on intracellular Ca2+, although this effect was smaller than that induced by the initial glucose treatment of the cells (Table 2).
Discussion
Our findings indicate that elevated d-glucose concentrations in PCAs directly stimulate the release of NO from the endothelial layer. This effect was due to the activity of eNOS and was associated with an increase in intracellular Ca2+. The response was specific to the monomeric d-stereoisomer of glucose and was not mediated by an increase in osmotic pressure, since equimolar concentrations of l-glucose failed to elevate either NO or intracellular Ca2+. Inhibition of NO release by Ni2+ or by the absence of extracellular Ca2+ demonstrates that Ca2+ entry from the extracellular space is the essential trigger for the activation of eNOS.
Since the coronary endothelium lacks voltage-gated Ca2+ channels [33], two possible pathways exist for calcium influx: receptor-activated Ca2+ channels and plasmalemmal transport proteins.
Involvement of Ca2+ channels can be excluded, as neither inhibition of capacitative calcium entry nor inhibition of Ca2+ influx via cAMP-dependent cation channels altered the stimulatory effects of d-glucose on NO formation. Hence, we propose that the influx of extracellular Ca2+ is the result of a transport process that is either directly or indirectly activated by d-glucose.
Two transporters are reportedly involved in the regulation of Ca2+-dependent eNOS activity, namely, PMCA and NCX. These proteins are localised in the plasmalemmal caveolae in close proximity to eNOS and participate in the control of sub-plasmalemmal intracellular Ca2+, which is of particular importance for modulation of eNOS activity [34, 35]. The high affinity/low capacity PMCA is the principal Ca2+ removal system in vascular endothelium [36]. However, failure of the PMCA- (and capacitative Ca2+ entry-) inhibitor La3+ to diminish d-glucose-mediated NO formation suggests that intracellular Ca2+ clearance by PMCA is not involved in glucose-dependent eNOS activation. In contrast, the complete abolition of d-glucose-induced increases in endothelial intracellular Ca2+ and NO release by inhibition of NCX indicates that stimulation of this protein is involved in the response to d-glucose. Previous reports have shown that Ca2+ extrusion by the low affinity/high capacity NCX system is triggered by intracellular Na+ loading [34]. Glucose cannot cross intact membranes by diffusion; its intracellular uptake is achieved by glucose transport systems. Passive entry via the ubiquitous transcellular d-glucose gradient-driven facilitative glucose transporters (GLUT1) is well characterised. Recently, an alternative secondary active uptake pathway via SGLT has been identified in the endothelium of several vascular beds [37, 38]. We hypothesised that elevation of the extracellular concentration of d-glucose would increase entry not only via GLUT1, but also via SGLT, leading to a rise in intracellular Na+ , which in turn stimulates Ca2+ uptake through NCX. This hypothesis is supported by the finding that the d-glucose-induced increase in intracellular Ca2+ and subsequent NO formation were completely blocked by the selective SGLT inhibitor phlorizin. The existence of functional SGLT in coronary artery endothelium is supported by the identification of SGLT-1 mRNA in aortic and coronary endothelium by RT-PCR in this study. It has been reported that GLUT1 and SGLT each contribute to approximately 50% of the glucose uptake in several vascular beds. Moreover, SGLT is rapidly desensitised by an increase in intracellular glucose concentrations [38]. Thus, selective inhibition of GLUT1 should delay desensitisation and therefore potentiate Na+ uptake via SGLT, triggering an increased Ca2+ and NO response. This explains the elevated magnitude and duration of the d-glucose-induced increase in endothelial intracellular Ca2+ and NO release in the presence of cytochalasin B.
As we made comparable observations using d-galactose instead of d-glucose we were able to exclude other members of this SGLT family (SGLT-2 and SGLT-3), since SGLT-1 does not discriminate between d-glucose and d-galactose, while neither SGLT-2 nor SGLT-3 transport d-galactose efficiently (Km >20 mmol/l) [31].
Although we have suggested a mechanism for glucose-induced endothelial NO release, the question remains whether this finding may be of physiological significance. A direct consequence of endothelial NO release is the relaxation of adjacent smooth muscle via activation of soluble guanylate cyclase. However, stimulation with high glucose alone had no effect on resting vascular tone. The apparent inability of high glucose to dilate coronary vessels may be explained by the relatively low magnitude of NO release. We recently reported that an increase in endothelial NO release of >5 nmol/l was required to trigger vasodilation [24]. Consistent with this finding, an elevated glucose-induced increase in NO of 5.7 nmol/l, achieved after inhibition of GLUT1, was sufficient to evoke relaxation. Moreover, we have demonstrated that the effect of the eNOS substrate L-arginine on NO release and vasodilation is enhanced by d-glucose in a concentration-dependent manner. This finding is in accordance with a report of Sobrevia et al. [39] which reported that d-glucose potentiates the uptake of l-arginine in vascular endothelial cells via the sodium-independent y+-transport system. However, this mechanism of eNOS activation may only be relevant at high levels of of L-arginine, and is unlikely to occur at physiological plasma concentrations with baseline levels of about 90 µmol/l and post-prandial peaks of about 130 µmol/l [40, 41].
In accordance with previous studies [42], the vasodilatory actions of insulin were confirmed to be endothelium-dependent, with eNOS activation mediated by receptor/tyrosine kinase, insulin receptor substrate (IRS-1), PI3K and serine/threonine protein kinase (Akt/PKB), but not Ca2+.
A key finding of our study is that the NO responses to insulin, as well as the relaxation responses, are potentiated by co-incubation with high d-glucose in a concentration-dependent fashion. The mechanism responsible for glucose-mediated amplification of the vascular response to insulin appears to be confined to SGLT- and NCX-activated, Ca2+-dependent eNOS stimulation, since inhibition of Ca2+ entry by inhibitors specific to Ni2+, SGLT or NCX completely abolished the additive glucose effect. We therefore conclude that an elevated plasma glucose level accelerates its own cellular uptake by NO-derived vasodilation, which is dependent on insulin- and glucose-stimulated endothelial NO formation.
The rapid clearance of glucose from the circulation also appears to be crucial for maintenance of endothelial function. Glucose/insulin-mediated vasodilation is impaired during hyperglycaemia: glucose-induced NO release was completely abolished and insulin-induced NO released was reduced after incubation of the PCAs at high glucose concentrations for 2 h. This finding may be explained by accelerated NO degradation due to enhanced superoxide generation in the chronic hyperglycaemic state [43]. However, during the relatively short periods (≤2 h) of incubation with high d-glucose in our experiments, we found no evidence of increased superoxide formation. Alternatively, it has been shown that insulin-induced PI3 K signalling pathways (which mediate endothelial NO release), GLUT4 translocation in skeletal muscle cells and adipocytes, as well as the metabolic actions of insulin, are impaired under conditions of prolonged hyperglycaemia, and are thus considered to constitute the molecular basis of insulin resistance [44, 45]. Additionally, NCX activity was found to be reduced in the high glucose state [46], whereas uptake of glucose by endothelial cells was not affected [47]. This may explain the failure of acute glucose addition to increase NO release after prolonged exposure to high glucose. A previous study demonstrated that improved glycaemic control by insulin infusion therapy partly restored insulin-stimulated endothelial function in patients with type 2 diabetes and ischaemic heart disease, highlighting the detrimental effects of persistent hyperglycaemia on PI3K-dependent signalling [48]. This is consistent with our observation that impaired vasodilatory function was only partly reversed by incubating PCAs previously compromised by high glucose in normoglycaemic buffer. Hence, it appears that the duration of hyperglycaemia determines the vascular response: while acute (post-prandial) hyperglycaemia enhances PI3K-mediated endothelium-dependent vasodilation, persistent hyperglycaemia causes a potentially irreversible impairment of glucose/insulin-mediated vasodilation, constituting an early hallmark of glucose- and insulin-resistance.
In summary, this is to our knowledge the first report to describe a d-glucose-stimulated NO release from intact vascular endothelium. We were able to resolve the mechanism for this effect, demonstrating that high extracellular d-glucose activates plasma membrane transporters associated with a net inward flux of Ca2+. Moreover, we found that high d-glucose potentiates the vasodilatory activity of insulin, suggesting that combined glucose- and insulin-mediated endothelial NO stimulation is implicated in the perfusion-dependent acceleration of glucose uptake, which in turn is essential for maintaining vascular endothelial function.
Abbreviations
- ddAdoPP:
-
2′,5′-dideoxyadenosine-3′-diphosphate
- eNOS:
-
endothelial isoform of nitric oxide synthase
- l-NMMA:
-
l-N G-monomethyl arginine
- NCX:
-
Na+/Ca2+ exchanger
- NO:
-
nitric oxide
- PAEC:
-
porcine aortic endothelial cell
- PCA:
-
porcine coronary conduit artery
- PI3K:
-
phosphatidylinositol 3′-OH kinase
- PMCA:
-
plasma membrane Ca2+ ATPase
- SERCA:
-
endoplasmic Ca2+ ATPase
- SGLT:
-
Na+/glucose cotransporter
References
Johnstone MT, Creager SJ, Scales KM, Cusco JA, Lee BK, Creager MA (1993) Impaired endothelium-dependent vasodilation in patients with insulin-dependent diabetes mellitus. Circulation 88:2510–2516
Williams SB, Cusco JA, Roddy MA, Johnstone MT, Creager MA (1996) Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 27:567–574
Noyman I, Marikovsky M, Sasson S et al. (2002) Hyperglycemia reduces nitric oxide synthase and glycogen synthase activity in endothelial cells. Nitric Oxide 7:187–193
Calles-Escandon J, Cipolla M (2001) Diabetes and endothelial dysfunction: a clinical perspective. Endocr Rev 22:36–52
Laakso M (1999) Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes 48:937–942
Haffner SM (1998) The importance of hyperglycemia in the nonfasting state to the development of cardiovascular disease. Endocr Rev 19:583–592
Tooke JE, Goh KL (1999) Vascular function in Type 2 diabetes mellitus and pre-diabetes: the case for intrinsic endotheiopathy. Diabet Med 16:710–715
Mitrakou A, Kelley D, Mokan M et al. (1992) Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N Engl J Med 326:22–29
Steinberg HO, Brechtel G, Johnson A, Fineberg N, Baron AD (1994) Insulin-mediated skeletal muscle vasodilation is nitric oxide dependent. A novel action of insulin to increase nitric oxide release. J Clin Invest 94:1172–1179
Scherrer U, Randin D, Vollenweider P, Vollenweider L, Nicod P (1994) Nitric oxide release accounts for insulin’s vascular effects in humans. J Clin Invest 94:2511–2515
Williams SB, Goldfine AB, Timimi FK et al. (1998) Acute hyperglycemia attenuates endothelium-dependent vasodilation in humans in vivo. Circulation 97:1695–1701
Renaudin C, Michoud E, Rapin JR, Lagarde M, Wiernsperger N (1998) Hyperglycaemia modifies the reaction of microvessels to insulin in rat skeletal muscle. Diabetologia 41:26–33
Kawano H, Motoyama T, Hirashima O et al. (1999) Hyperglycemia rapidly suppresses flow-mediated endothelium-dependent vasodilation of brachial artery. J Am Coll Cardiol 34:146–154
Title LM, Cummings PM, Giddens K, Nassar BA (2000) Oral glucose loading acutely attenuates endothelium-dependent vasodilation in healthy adults without diabetes: an effect prevented by vitamins C and E. J Am Coll Cardiol 36:2185–2191
Beckman JA, Goldfine AB, Gordon MB, Creager MA (2001) Ascorbate restores endothelium-dependent vasodilation impaired by acute hyperglycemia in humans. Circulation 103:1618–1623
Kim SH, Park KW, Kim YS et al. (2003) Effects of acute hyperglycemia on endothelium-dependent vasodilation in patients with diabetes mellitus or impaired glucose metabolism. Endothelium 10:65–70
Cipolla MJ, Porter JM, Osol G, Mayhan WG (1997) High glucose concentrations dilate cerebral arteries and diminish myogenic tone through an endothelial mechanism. Stroke 28:405–411
van Veen S, Frolich M, Chang PC (1999) Acute hyperglycaemia in the forearm induces vasodilation that is not modified by hyperinsulinaemia. J Hum Hypertens 13:263–268
Hoffman RP, Hausberg M, Sinkey CA, Anderson EA (1999) Hyperglycemia without hyperinsulinemia produces both sympathetic neural activation and vasodilation in normal humans. J Diabetes Complications 13:17–22
Oomen PH, Kant GD, Dullaart RP, Reitsma WD, Smit AJ (2002) Acute hyperglycemia and hyperinsulinemia enhance vasodilatation in Type 1 diabetes mellitus without increasing capillary permeability and inducing endothelial dysfunction. Microvasc Res 63:1–9
Houben AJ, Schaper NC, de Haan CH et al. (1996) Local 24-h hyperglycemia does not affect endothelium-dependent or -independent vasoreactivity in humans. Am J Physiol 270:H2014–H2020
Brands MW, Fitzgerald SM (1998) Acute endothelium-mediated vasodilation is not impaired at the onset of diabetes. Hypertension 32:541–547
Charkoudian N, Vella A, Reed AS et al. (2002) Cutaneous vascular function during acute hyperglycemia in healthy young adults. J Appl Physiol 93:1243–1250
Taubert D, Berkels R, Klaus W, Roesen R (2002) Nitric oxide formation and corresponding relaxation of porcine coronary arteries induced by plant phenols: essential structural features. J Cardiovasc Pharmacol 40:701–713
Berkels R, Mueller A, Roesen R, Klaus W (1999) Nifedipine and Bay K 8644 induce an increase of [Ca2+]i and nitric oxide in endothelial cells. J Cardiovasc Pharmacol Ther 4:175–181
Grynkiewicz G, Poenie M, Tsien RY (1985) A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260:3440–3450
Edgell CJ, McDonald CC, Graham JB (1983) Permanent cell line expressing human factor VIII-related antigen established by hybridization. Proc Natl Acad Sci USA 80:3734–3737
Chomczynski P, Sacchi N (1987) Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162:156–159
Wang X, Reznick S, Li P, Liang W, van Breemen C (2002) Ca2+ removal mechanisms in freshly isolated rabbit aortic endothelial cells. Cell Calcium 31:265–277
Bell GI, Burant CF, Takeda J, Gould GW (1993) Structure and function of mammalian facilitative sugar transporters. J Biol Chem 268:19161–19164
Wright EM (2001) Renal Na+-glucose cotransporters. Am J Physiol Renal Physiol 280:F10–F18
Ohta T, Isselbacher KJ, Rhoads DB (1990) Regulation of glucose transporters in LLC-PK1 cells: effects of d-glucose and monosaccharides. Mol Cell Biol 10:6491–6499
Uchida H, Tanaka Y, Ishii K, Nakayama K (1999) l-type Ca2+ channels are not involved in coronary endothelial Ca2+ influx mechanism responsible for endothelium-dependent relaxation. Res Commun Mol Pathol Pharmacol 104:127–144
Teubl M, Groschner K, Kohlwein SD, Mayer B, Schmidt K (1999) Na(+)/Ca(2+) exchange facilitates Ca2+-dependent activation of endothelial nitric-oxide synthase. J Biol Chem 274:29529–29535
Schneider JC, El Kebir D, Chereau C, Mercier JC, Dall’Ava-Santucci J, Dinh-Xuan AT (2002) Involvement of Na+/Ca2+ exchanger in endothelial NO production and endothelium-dependent relaxation. Am J Physiol Heart Circ Physiol 283:H837–H844
Sedova M, Blatter LA (1999) Dynamic regulation of [Ca2+]i by plasma membrane Ca2+-ATPase and Na+/Ca2+ exchange during capacitative Ca2+ entry in bovine vascular endothelial cells. Cell Calcium 25:333–343
Nishizaki T, Kammesheidt A, Sumikawa K, Asada T, Okada Y (1995) A sodium- and energy-dependent glucose transporter with similarities to SGLT1–2 is expressed in bovine cortical vessels. Neurosci Res 22:13–22
Nishizaki T, Matsuoka T, Kammesheidt A, Sumikawa K, Asada T, Okada Y (1998) Low glucose enhances Na+/glucose transport in bovine brain artery endothelial cells. Stroke 29:844–849
Sobrevia L, Nadal A, Yudilevich DL, Mann GE (1996) Activation of l-arginine transport (system y+) and nitric oxide synthase by elevated glucose and insulin in human endothelial cells. J Physiol 490:775–781
Tangphao O, Chalon S, Coulston AM et al. (1999) l-arginine and nitric oxide-related compounds in plasma: comparison of normal and arginine-free diets in a 24-h crossover study. Vasc Med 4:27–32
Tangphao O, Grossmann M, Chalon S, Hoffman BB, Blaschke TF (1999) Pharmacokinetics of intravenous and oral l-arginine in normal volunteers. Br J Clin Pharmacol 47:261–266
Montagnani M, Chen H, Barr VA, Quon MJ (2001) Insulin-stimulated activation of eNOS is independent of Ca2+ but requires phosphorylation by Akt at Ser(1179). J Biol Chem 276:30392–30398
Cosentino F, Hishikawa K, Katusic ZS, Luscher TF (1997) High glucose increases nitric oxide synthase expression and superoxide anion generation in human aortic endothelial cells. Circulation 96:25–28
Zierath JR, Krook A, Wallberg-Henriksson H (2000) Insulin action and insulin resistance in human skeletal muscle. Diabetologia 43:821–835
Steinberg HO, Baron AD (2002) Vascular function, insulin resistance and fatty acids. Diabetologia 45:623–634
Hattori Y, Matsuda N, Kimura J et al. (2000) Diminished function and expression of the cardiac Na+-Ca2+ exchanger in diabetic rats: implication in Ca2+ overload. J Physiol 527:85–94
Vinals F, Gross A, Testar X, Palacin M, Rosen P, Zorzano A (1999) High glucose concentrations inhibit glucose phosphorylation, but not glucose transport, in human endothelial cells. Biochim Biophys Acta 1450:119–129
Rask-Madsen C, Ihlemann N, Krarup T et al. (2001) Insulin therapy improves insulin-stimulated endothelial function in patients with type 2 diabetes and ischemic heart disease. Diabetes 50:2611–2618
Poppe R, Karbach U, Gambaryan S et al. (1997) Expression of the Na+-d-glukose cotransporter SGLT1 in neurons. J Neurochem 69:84–94
Acknowledgements
We thank K. Helfert for skilful technical assistance. The authors are not aware of any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taubert, D., Rosenkranz, A., Berkels, R. et al. Acute effects of glucose and insulin on vascular endothelium. Diabetologia 47, 2059–2071 (2004). https://doi.org/10.1007/s00125-004-1586-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1586-1