Abstract
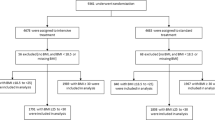
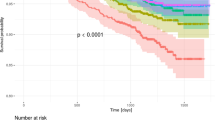
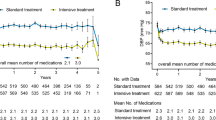
SPRINT is the first randomized, controlled trial showing that a systolic blood-pressure goal of <120 mmHg can be attained with cardiovascular benefits in a select group of patients with hypertension and an elevated cardiovascular risk with different origins. Although the patient population with characteristics like those in SPRINT makes up only 20–30% of the total hypertensive population, SPRINT is a landmark study that highlights the need to consider lower blood- pressure goals in the treatment of hypertension. Extending this study to include other patient populations and geographical areas is the next step for evaluating the benefits of strict blood-pressure targets and the generalizability of the SPRINT results. Importantly, the blood-pressure measurement method used in SPRINT differs from previous clinical trials, and raises the issue of whether a more accurate method should be used in clinical trials and if such method is feasible in clinical practice. This Perspectives article provides an analysis of the SPRINT data, focusing on patient characteristics, blood-pressure measurement method, and applicability of the SPRINT findings for future management guidelines.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ezzati, M. et al. Selected major risk factors and global and regional burden of disease. Lancet 360, 1347–1360 (2002).
GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–1724 (2016).
Lawes, C. M., Vander Hoorn, S., Rodgers, A. & International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 371, 1513–1518 (2008).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Mancia, G. et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 34, 2159–2219 (2013).
FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and other Tools) Resource. NCBI https://www.ncbi.nlm.nih.gov/books/NBK326791/ (2016).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311, 507–520 (2014).
Weber, M. A. et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J. Clin. Hypertens. (Greenwich) 16, 14–26 (2014).
National Institute for Health and Clinical Excellence. Hypertension in adults: diagnosis and management: clinical guideline [CG127]. NICE http://guidance.nice.org.uk/cg127 (2011).
Yusuf, S. Unresolved issues in the management of hypertension. Hypertension 55, 832–834 (2010).
Diao, D., Wright, J. M., Cundiff, D. K. & Gueyffier, F. Pharmacotherapy for mild hypertension. Cochrane Database Syst. Rev. 8, CD006742 (2012).
Sundström, J. et al. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet 384, 591–598 (2014).
Sundström, J. et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann. Intern. Med. 162, 184–191 (2015).
Thomopoulos, C., Parati, G. & Zanchetti, A. Effects of blood-pressure-lowering treatment in hypertension: 9. Discontinuations for adverse events attributed to different classes of antihypertensive drugs: meta-analyses of randomized trials. J. Hypertens. 34, 1921–1932 (2016).
Thomopoulos, C., Parati, G. & Zanchetti, A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more versus less intensive blood pressure lowering and different achieved blood pressure levels — updated overview and meta-analyses of randomized trials. J. Hypertens. 34, 613–622 (2016).
Xie, X. et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 387, 435–443 (2016).
Weber, M. A. et al. Systolic blood pressure and cardiovascular outcomes during treatment of hypertension. Am. J. Med. 126, 501–508 (2013).
Okin, P. M., Hille, D. A., Kjeldsen, S. E., Dahlöf, B. & Devereux, R. B. Impact of lower achieved blood pressure on outcomes in hypertensive patients. J. Hypertens. 30, 802–810 (2012).
The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Egan, B. M. & Stevens-Fabry, S. Prehypertension — prevalence, health risks, and management strategies. Nat. Rev. Cardiol. 12, 289–300 (2015).
Estruch, R., Ros, E. & Martínez-González, M. A. Mediterranean diet for primary prevention of cardiovascular disease. N. Engl. J. Med. 369, 676–677 (2013).
Banegas, J. R. et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur. Heart J. http://dx.doi.org/10.1093/eurheartj/ehu016 (2014).
Kjeldsen, S. E., Narkiewicz, K., Hedner, T. & Mancia, G. The SPRINT study: outcome may be driven by difference in diuretic treatment demasking heart failure and study design may support systolic blood pressure target below 140 mm Hg rather than below 120 mm Hg. Blood Press. 25, 63–66 (2016).
Touyz, R. M. & Dominiczak, A. F. Successes of SPRINT, but still some hurdles to cross. Hypertension 67, 268–269 (2016).
Williamson, J. D. et al. Intensive versus standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 315, 2673–2682 (2016).
Yusuf, S. et al. Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N. Engl. J. Med. 374, 2032–2043 (2016).
Cushman, W. C. et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 362, 1575–1585 (2010).
Sarafidis, P. A., Lazaridis, A. A., Ruiz-Hurtado, G. & Ruilope, L. M. Blood pressure reduction in diabetes: lessons from ACCORD, SPRINT and EMPA-REG OUTCOME. Nat. Rev. Endocrinol. http://dx.doi.org/10.1038/nrendo.2016.209 (2017).
Cohen, D. L. & Townsend, R. R. Which patients does the SPRINT study not apply to and what are the appropriate blood pressure goals in these populations? J. Clin. Hypertens. (Greenwich) 18, 477–478 (2016).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373, 2117–2128 (2015).
Bress, A. P. et al. Generalizability of SPRINT results to the U.S. adult population. J. Am. Coll. Cardiol. 67, 463–472 (2016).
de la Sierra, A. et al. Ambulatory blood pressure in hypertensive patients with inclusion criteria for the SPRINT trial. J. Am. Soc. Hypertens. 10, 947–953.e5 (2016).
Drawz, P. E. et al. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) ambulatory blood pressure study. Hypertension 69, 42–50 (2017).
Parati, G., Ochoa, J. E., Bilo, G. & Zanchetti, A. SPRINT blood pressure: sprinting back to Smirk's basal blood pressure? Hypertension 69, 15–19 (2017).
Myers, M. G. A. Short history of automated office blood pressure — 15 years to SPRINT. J. Clin. Hypertens. (Greenwich) 18, 721–724 (2016).
Banegas, J. R. et al. Clinic versus daytime ambulatory blood pressure difference in hypertensive patients: the impact of age and clinic blood pressure. Hypertension 69, 211–219 (2017).
Schwartz, J. E. et al. Clinic blood pressure underestimates ambulatory blood pressure in an untreated employer-based US population: results from the Masked Hypertension Study. Circulation 134, 1794–1807 (2016).
Myers, M. G. et al. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension 55, 195–200 (2010).
Filipovský, J. et al. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 25, 228–234 (2016).
Kjeldsen, S. E., Lund-Johansen, P., Nilsson, P. M. & Mancia, G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension 67, 808–812 (2016).
Ruilope, L. M. SPRINT. Counteracting the risk of prehypertension? J. Am. Soc. Hypertens. 10, 546–547 (2016).
Egan, B. M., Li, J. & Wagner, C. S. Systolic Blood Pressure Intervention Trial (SPRINT) and target systolic blood pressure in future hypertension guidelines. Hypertension 68, 318–323 (2016).
Pocock, S. J. & Stone, G. W. The primary outcome is positive — is that good enough? N. Engl. J. Med. 375, 971–979 (2016).
Thomas, F., Pannier, B. & Safar, M. E. Impact of country of birth on progression of steady and pulsatile hemodynamic parameters in normotensive and hypertensive subjects. J. Am. Soc. Hypertens. 7, 440–447 (2013).
Lieber, A. et al. Cardiovascular prevention: relationships between arterial aging and chronic drug treatment. J. Hum. Hypertens. 25, 524–531 (2011).
Leung, A. A. et al. Hypertension Canada's 2016 Canadian hypertension education program guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can. J. Cardiol. 32, 569–588 (2016).
National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults. Heart Foundation https://www.heartfoundation.org.au/images/uploads/publications/PRO-167_Hypertension-guideline-2016_WEB.pdf (2016).
López-Jaramillo, P., Coca, A., Sánchez, R., Zanchetti, A. & Latin American Society of Hypertension. Hypertension guidelines: is it time to reappraise blood pressure thresholds and targets? Position Statement of the Latin American Society of Hypertension. Hypertension 68, 257–262 (2016).
Acknowledgements
Specific funding for this study was obtained from FIS ISCIII grants PI13/02321, PI16/01460, PIE13/00045, PI14/01841, CP15/0129, CIBERCV, Fundación SENEFRO/SEN, and Fondo Europeo de Desarrollo Regional FEDER and FSE.
Author information
Authors and Affiliations
Contributions
G.R.-H., J.R.B., and L.M.R. researched data for the article and wrote the manuscript. All authors provided substantial contribution to the discussion of content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Ruiz-Hurtado, G., Banegas, J., Sarafidis, P. et al. Has the SPRINT trial introduced a new blood-pressure goal in hypertension?. Nat Rev Cardiol 14, 560–565 (2017). https://doi.org/10.1038/nrcardio.2017.74
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2017.74
This article is cited by
-
Applying systems thinking to unravel the mechanisms underlying orthostatic hypotension related fall risk
GeroScience (2023)
-
Highlights of ESC/ESH 2018 Guidelines on the Management of Hypertension: What Every Doctor Should Know
High Blood Pressure & Cardiovascular Prevention (2019)
-
Ambulatory versus clinic BP values
Nature Reviews Cardiology (2018)
-
The optimal blood pressure target in diabetes mellitus: a quest coming to an end?
Journal of Human Hypertension (2018)
-
Which Target Blood Pressure in Year 2018? Evidence from Recent Clinical Trials
High Blood Pressure & Cardiovascular Prevention (2018)