ABSTRACT
INTRODUCTION
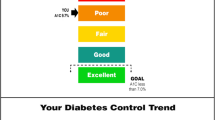
Previous work has indicated that for patients with diabetes, there is value in understanding glycemic control. Despite these findings, patient understanding of the hemoglobin A1C value (A1C) is notably poor. In this study, we test the effect of two alternative communication formats of the A1C on improving glycemic control among patients with poorly controlled diabetes.
METHODS
177 patients with poorly controlled diabetes were randomized to one of three study arms that varied in the information they received: (1) a “diabetes report card” containing individualized information about glycemic control for each participant with letter grades ranging from A to F; (2) a “report card” containing a face whose emotion reflected current glycemic control; or (3) a “report card” with glycemic control expressed with the A1C value (standard arm). The primary study outcome was change in A1C at 6 months. Secondary outcomes included changes in participant perceptions of their glycemic control.
RESULTS
The average A1C for enrolled participants was 9.9 % (S.D. 1.7) and did not differ significantly among study arms. We noted no significant differences in change in A1C at 6 months between the standard and experimental arms. Using multiple imputation to account for missing A1C values, the changes in A1C for the letter grade, face, and standard arms were -0.55 % (-1.15, 0.05), -0.89 % (-1.49, -0.29), and -0.74 % (-1.51, 0.029), respectively (p = 0.67 for control vs. grade, p = 0.76 for control vs. face).
DISCUSSION
Feedback to patients with poorly controlled diabetes in the form of letter grades and faces did not differentially impact glycemic control at 6 months or participant perceptions of current control. These efforts to improve communication and patient understanding of disease management targets need further refinement to significantly impact diabetes outcomes.
Clinical Trial ID
NCT01143870


Similar content being viewed by others
REFERENCES
Schillinger D, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–82.
Beard E, et al. Do people with diabetes understand their clinical marker of long-term glycemic control (HbA1c levels) and does this predict diabetes self-care behaviours and HbA1c? Patient Educ Couns. 2010;80:227–32.
Berikai P, et al. Gain in patients’ knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care. 2007;30(6):1587–9.
Wang S, et al. Lack of knowledge of glycosylated hemoglobin in patients with diabetic retinopathy. Diabetes Res Clin Pract. 2008;81(1):e15–7.
HealthBoards.com. Available from: http://www.healthboards.com/boards/diabetes/909152-doctor-confused-so-am-i-good-a1c-high-bs.html. Accessed 13 Jan 2014.
DiabetesDaily.com. Available from: http://www.diabetesdaily.com/forum/type-2-diabetes/29602-a1c-confusion-help/. Acessed 13 Jan 2014
Parkes G, et al. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008;336(7644):598–600.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175–83.
American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012;35(Supplement 1):S11–63.
New York City Department of Health and Mental Hygiene. Available from: http://www.nyc.gov/html/doh/html/services/restaurant-inspection.shtml. Accessed 13 Jan 2014.
The Leapfrog Group. Available from: http://www.hospitalsafetyscore.org/. Accessed 13 Jan 2014.
Wong DL, Hokenberry-Eaton M, Wilson D, Winkelstein ML, Schwartz P. Wong’s Essentials of Pediatric Nursing. 6th ed. Saint Louis: Mosby Inc; 2001.
Kaufman L. Utilities Turn Their Customers Green, With Envy, in The New York Times. New York: The New York Times Company; 2009.
Cavanaugh K, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–46.
Osborn CY, et al. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009;32(9):1614–9.
Schwartz LM, et al. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127(11):966–72.
Nathan DM, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29(8):1963–72.
Molyneaux LM, et al. Better glycaemic control and risk reduction of diabetic complications in Type 2 diabetes: comparison with the DCCT. Diabetes Res Clin Pract. 1998;42(2):77–83.
The Diabetes Control and Complications Trial Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995; 44(8):968–83.
Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: John Wiley & Sons, Inc; 1987.
Long JA, et al. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med. 2012;156(6):416–24.
Lorincz IS, Lawson BC, Long JA. Provider and patient directed financial incentives to improve care and outcomes for patients with diabetes. Curr Diab Rep. 2013;13(2):188–95.
Volpp KG, et al. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–7.
Ratanawongsa N, et al. Communication and medication refill adherence: the diabetes study of Northern California. Arch Intern Med. 2012; 1–9.
Acknowledgements
Authors
All authors listed on the title page met the criterion for authorship based on the Committee on Publication Ethics guidelines.
Contributorship
Cathy Bryan assisted with participant recruitment and enrollment, Dr. Mark Wiener, and Alice Livshits assisted with use of the E.M.R. and tracking of participant outcomes, and Yuanyuan Tao helped with exploratory data analysis.
Funding
Penn CMU Roybal P30 Center Grant P30AG034546. The funder was not involved in any part of the study design, conducting of the study or the analysis of the results.
Prior Presentations
This work was presented as an oral abstract at the 2013 Society of General Internal Medicine Annual Meeting.
Competing Interests
Several members of the research team and the submitted work were supported by grant funds from the Penn CMU Roybal P30, a non-profit entity; no member of the research team had any financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; there are no other relationships or activities that may have otherwise influenced the submitted work.
Ethical Approval
The study protocol was approved by the University of Pennsylvania Institutional Review Board.
Data Sharing
No additional data available.
Peer Review
Not commissioned, externally peer-reviewed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gopalan, A., Tahirovic, E., Moss, H. et al. Translating the Hemoglobin A1C with More Easily Understood Feedback: A Randomized Controlled Trial. J GEN INTERN MED 29, 996–1003 (2014). https://doi.org/10.1007/s11606-014-2810-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2810-4