Abstract
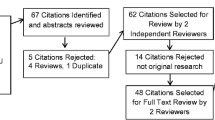
The Diabetes Prevention Program (DPP), an evidenced-based lifestyle intervention for type 2 diabetes (T2D), has been translated for use with ethnic minority communities throughout the United States that are disproportionately at-risk for T2D. The present paper sought to critically review ethnic translation studies of the DPP with respect to translation methods utilized, the success of these methods, and alternative or supplemental methodologies for future translation efforts. Manuscripts reviewed were found by searching PubMed and PsycINFO, using the terms: “diabetes prevention program” AND [“translation” or “ethnic”]. Of 89 papers found, only 6 described ethnic translations of the DPP in the United States, and were included in this review. Translations of the DPP to African American, Hispanic/Latino, Native Hawaiian and Other Pacific Islander, Arab American, and American Indian and Native Alaskan communities were identified and reviewed. The most common translation strategies included group-based delivery and use of bilingual study personnel. Generally, these factors appeared to increase acceptability of the intervention within the ethnic communities reviewed, and should be considered in future efforts to implement and translate the DPP to ethnic communities in the United States.
Similar content being viewed by others
References
Eriksson KF, Lindgärde F. Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. The 6-year Malmö feasibility study. Diabetologia. 1991;34(12):891–8.
Pan X-R, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–44.
Ramachandran A, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–97.
Tuomilehto J, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Supplement 1):S67–74.
Neel JV. Diabetes mellitus—a thrifty genotype rendered detrimental by progress. Am J Hum Genet. 1962;14(4):353–1000.
Rejeski WJ, et al. Correlates of health-related quality of life in overweight and obese adults with type 2 diabetes. Obesity. 2012;14(5):870–83.
Brower V. Illuminating the diabetes–cancer link. J Natl Cancer Inst. 2012;104(14):1048–50.
Danaei G, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2· 7 million participants. Lancet. 2011;378(9785):31–40.
Cowie CC, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the US population in 1988–2006. Diabetes Care. 2010;33(3):562–8.
Mayer-Davis EJ, et al. The many faces of diabetes in American youth: type 1 and type 2 diabetes in five race and ethnic populations: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(Supplement 2):S99–101.
Steyn NP, et al. Diet, nutrition and the prevention of type 2 diabetes. Public Health Nutr. 2004;7(1A; SPI):147–66.
Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. U.S. Department of Health and Human Services. 2011.
Alberti KGMM, et al. International Diabetes Federation: a consensus on type 2 diabetes prevention. Diabet Med. 2007;24(5):451–63.
Hu FB, et al. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289(14):1785–91.
Hu FB, et al. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med. 2001;161(12):1542.
Steyn NP, et al. Nutrition interventions for the prevention of type 2 diabetes. Proc Nutr Soc. 2009;68(01):55–70.
Knowler WC, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Knowler WC, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86.
Cardona-Morrell M, et al. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC Public Health. 2010;10(1):653.
Whittemore R. A systematic review of the translational research on the Diabetes Prevention Program. Transl Behav Med. 2011;1(3):480–91.
Boltri JM, et al. Diabetes prevention in a faith-based setting: results of translational research. J Public Health Manag Pract. 2008;14(1):29–32.
Merriam PA, et al. Methodology of a diabetes prevention translational research project utilizing a community-academic partnership for implementation in an underserved Latino community. BMC Med Res Methodol. 2009;9(1):20.
Mau MK, et al. Translating diabetes prevention into native Hawaiian and Pacific Islander communities: the PILI ‘Ohana Pilot project. Prog Community Health Partnersh Res Educ Action. 2010;4(1):7–16.
Jaber LA, et al. Feasibility of group lifestyle intervention for diabetes prevention in Arab Americans. Diabetes Res Clin Pract. 2011;91(3):307–15.
Jiang L, et al. Translating the Diabetes Prevention Program into American Indian and Alaska Native Communities Results from the Special Diabetes Program for Indians Diabetes Prevention Demonstration Project. Diabetes Care. 2013;36(7):2027–34.
Boltri JM, et al. Translation of the National Institutes of Health Diabetes Prevention Program in African American churches. J Natl Med Assoc. 2011;103(3):194–202.
Hoyo C, et al. Program prioritization to control chronic diseases in African-American faith-based communities. J Natl Med Assoc. 2004;96(4):524–32.
Gallup. Asian-Americans lean left politically. 2010. http://www.gallup.com/poll/125579/asian-americans-lean-leftpolitically.aspx. Accessed 10 Oct 2012.
Anderson-Loftin W, et al. Soul food light culturally competent diabetes education. Diabetes Educ. 2005;31(4):555–63.
Airhihenbuwa CO, et al. Cultural aspects of African American eating patterns. Ethn Health. 1996;1(3):245–60.
Hawkins RP, et al. Understanding tailoring in communicating about health. Health Educ Res. 2008;23(3):454–66.
Belza B, et al. Older adult perspectives on physical activity and exercise: voices from multiple cultures. Prev Chronic Dis. 2004;1(4):1–12.
U.S. Census Bureau. American Community Survey: 3-year estimates. 2011. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_3YR_S0201&prodType=table. Accessed 25 Nov 2012.
Narayan KM, et al. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884–90.
Lara M, et al. Acculturation and Latino health in the United States. In: LaVeist TA, Isaac LA, editors. Race, ethnicity, and health: a public health reader. Wiley; 2012.
Moreno G, Morales LS. Hablamos Juntos (together we speak): interpreters, provider communication, and satisfaction with care. J Gen Intern Med. 2010;25(12):1282–8.
Noar SM, et al. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–93.
Abraído-Lanza AF, et al. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61(6):1243–55.
Melillo K, et al. Perceptions of older Latino adults regarding physical fitness, physical activity, and exercise. J Gerontol Nurs. 2001;27(9):38–46.
Shaibi GQ, et al. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006;38(7):1208–15.
Grandinetti A, et al. Prevalence of glucose intolerance among Native Hawaiians in two rural communities. Diabetes Care. 1998;21(4):549–54.
Florentina R, et al. 2001–2003 State of Hawaii by Ethnicity—Hawaiian behavioral risk factor surveillance system. Honolulu: Health HSDo; 2004.
Ford JG, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008;112(2):228–42.
Kaholokula JKA, et al. Native and Pacific health disparities research. Hawaii Med J. 2008;67(8):218.
Wing R, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145–54.
Kaopua LSI, et al. Testing the feasibility of a culturally tailored breast cancer screening intervention with Native Hawaiian women in rural churches. Health Soc Work. 2011;36(1):55–65.
Jaber LA, et al. Epidemiology of diabetes among Arab Americans. Diabetes Care. 2003;26(2):308–13.
Rosenstock IM, et al. Social learning theory and the health belief model. Health Educ Behav. 1988;15(2):175–83.
Erickson CD, Al-Timimi NR. Providing mental health services to Arab Americans: recommendations and considerations. Cult Divers Ethn Minor Psychol. 2001;7(4):308–27.
Israel BA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202.
Baxter J, et al. Differences in recruitment and early retention among ethnic minority participants in a large pediatric cohort: the TEDDY Study. Contemp Clin Trials. 2012;33(4):633–40.
Ackermann RT, et al. An evaluation of cost sharing to finance a diet and physical activity intervention to prevent diabetes. Diabetes Care. 2006;29(6):1237–41.
Elbert NJ, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16(4):e110.
Webb MS, et al. Tailored interventions for motivating smoking cessation: using placebo tailoring to examine the influence of expectancies and personalization. Health Psychol. 2005;24(2):179–88.
Sorkin DH, Mavandadi S, Rook KS, Biegler KA, Kilgore D, Dow E, Ngo-Metzger Q. Dyadic collaboration in shared health behavior change: the effects of a randomized trial to test a lifestyle intervention for high-risk Latinas. Health Psychol. 2014;33(6):566–75.
Shai I, Jiang R, Manson JE, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–90.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hall, D.L., Lattie, E.G., McCalla, J.R. et al. Translation of the Diabetes Prevention Program to Ethnic Communities in the United States. J Immigrant Minority Health 18, 479–489 (2016). https://doi.org/10.1007/s10903-015-0209-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-015-0209-x