Abstract
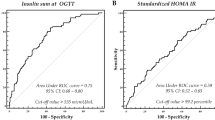
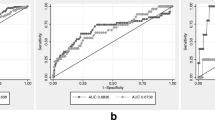
Type 2 diabetes can occur without any symptoms, and health problems associated with the disease are serious. Screening tests allowing an early diagnosis are desirable. However, optimal screening tests for diabetes in obese youth are discussed controversially. We performed an observational multicenter analysis including 4848 (2668 female) overweight and obese children aged 7 to 17 years without previously known diabetes. Using HbA1c and OGTT as diagnostic criteria, 2.4% (n = 115, 55 female) could be classified as having diabetes. Within this group, 68.7% had HbA1c levels ≥48 mmol/mol (≥6.5%). FPG ≥126 mg/dl (≥7.0 mmol/l) and/or 2-h glucose levels ≥200 mg/dl (≥11.1 mmol/l) were found in 46.1%. Out of the 115 cases fulfilling the OGTT and/or HbA1c criteria for diabetes, diabetes was confirmed in 43.5%. For FPG, the ROC analysis revealed an optimal threshold of 98 mg/dl (5.4 mmol/l) (sensitivity 70%, specificity 88%). For HbA1c, the best cut-off value was 42 mmol/mol (6.0%) (sensitivity 94%, specificity 93%).
Conclusions: HbA1c seems to be more reliable than OGTT for diabetes screening in overweight and obese children and adolescents. The optimal HbA1c threshold for identifying patients with diabetes was found to be 42 mmol/mol (6.0%).
What is Known: • The prevalence of obesity is increasing and health problems related to type 2 DM can be serious. However, an optimal screening test for diabetes in obese youth seems to be controversial in the literature. |
What is New: • In our study, the ROC analysis revealed for FPG an optimal threshold of 98 mg/dl (5.4 mmol/l, sensitivity 70%, specificity 88%) and for HbA1c a best cut-off value of 42 mmol/mol (6.0%, sensitivity 94%, specificity 93%) to detect diabetes. Thus, in overweight and obese children and adolescents, HbA1c seems to be a more reliable screening tool than OGTT. |


Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- FPG:
-
Fasting plasma glucose
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- OGTT:
-
Oral glucose tolerance test
- SDS:
-
Standard deviation score
References
American Diabetes Association (2015) (2) Classification and diagnosis of diabetes. Diabetes Care 38(Suppl. 1):S8–S16
Arbeitsgemeinschaft Adipositas im Kindes- und Jugendalter (2014) Konsensbasierte (S2) Leitlinie zur Diagnostik, Therapie und Prävention von Übergewicht und Adipositas im Kindes- und Jugendalter. Available at http://www.aga.adipositas-gesellschaft.de/index.php?id=9. Accessed 05 Nov 2015
Bennett CM, Guo M, Dharmage SC (2007) HbA(1c) as a screening tool for detection of Type 2 diabetes: a systematic review. Diabet Med 24:333–343
Berhan YT, Mollsten A, Carlsson A, Hogberg L, Ivarsson A, Dahlquist G (2014) Five-region study finds no evidence of undiagnosed type 2 diabetes in Swedish 11- to 13-year-olds. Acta Paediatr 103:1078–1082
Brar PC, Mengwall L, Franklin BH, Fierman AH (2014) Screening obese children and adolescents for prediabetes and/or type 2 diabetes in pediatric practices: a validation study. Clin Pediatr (Phila) 53:771–776
Buse JB, Kaufman FR, Linder B, Hirst K, El Ghormli L, Willi S, HEALTHY Study Group (2013) Diabetes screening with hemoglobin A(1c) versus fasting plasma glucose in a multiethnic middle-school cohort. Diabetes Care 36:429–435
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240–1243
Droumaguet C, Balkau B, Simon D, Caces E, Tichet J, Charles MA, Eschwege E, DESIR Study Group (2006) Use of HbA1c in predicting progression to diabetes in French men and women: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 29:1619–1625
Ehehalt S, Neu A (2011) Insulin resistance in childhood and adolescence. In: Ranke MB, Mullis PE (eds) Diagnostics of endocrine function in children and adolescents, 4th edn. Karger, Basel, pp. 294–309
Ehtisham S, Hattersley AT, Dunger DB, Barrett TG, British Society for Paediatric Endocrinology and Diabetes Clinical Trials Group (2004) First UK survey of paediatric type 2 diabetes and MODY. Arch Dis Child 89:526–529
Hagman E, Reinehr T, Kowalski J, Ekbom A, Marcus C, Holl RW (2014) Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int J Obes 38:40–45
Herdzik E, Safranow K, Ciechanowski K (2002) Diagnostic value of fasting capillary glucose, fructosamine and glycosylated haemoglobin in detecting diabetes and other glucose tolerance abnormalities compared to oral glucose tolerance test. Acta Diabetol 39:15–22
Jesudason DR, Dunstan K, Leong D, Wittert GA (2003) Macrovascular risk and diagnostic criteria for type 2 diabetes: implications for the use of FPG and HbA(1c) for cost-effective screening. Diabetes Care 26:485–490
Kapadia C, Zeitler P, Drugs and Therapeutics Committee of the Pediatric Endocrine Society (2012) Hemoglobin A1c measurement for the diagnosis of Type 2 diabetes in children. Int J Pediatr Endocrinol 2012:31
Kester LM, Hey H, Hannon TS (2012) Using hemoglobin A1c for prediabetes and diabetes diagnosis in adolescents: can adult recommendations be upheld for pediatric use? J Adolesc Health 50:321–323
Kleber M, Lass N, Papcke S, Wabitsch M, Reinehr T (2010) One-year follow-up of untreated obese white children and adolescents with impaired glucose tolerance: high conversion rate to normal glucose tolerance. Diabet Med 27:516–521
Ko GT, Chan JC, Yeung VT, Chow CC, Tsang LW, Li JK, So WY, Wai HP, Cockram CS (1998) Combined use of a fasting plasma glucose concentration and HbA1c or fructosamine predicts the likelihood of having diabetes in high-risk subjects. Diabetes Care 21:1221–1225
Körner A, Wiegand S, Hungele A, Tuschy S, Otto KP, l'Allemand-Jander D, Widhalm K, Kiess W, Holl RW, APV initiative, German Competence Net Obesity (2013) Longitudinal multicenter analysis on the course of glucose metabolism in obese children. Int J Obes 37:931–936
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V, von Hippel A, Jaeger U, Johnsen D, Korte W, Menner K, Müller G, Müller JM, Niemann-Pilatus A, Remer T, Schaefer F, Wittchen HU, Zabransky S, Zellner K, Ziegler A, Hebebrand J (2001) Perzentile für den Body-Mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschr Kinderheilk 149:807–818
Kromeyer-Hauschild K (2005) Definition, Anthropometrie und deutsche Referenzwerte für BMI. In: Wabitsch M, Hebebrand J, Kiess W, Zwiauer K (eds) Adipositas bei Kindern und Jugendlichen. Springer, Berlin, Heidelberg, pp. 9–10
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL (2002) CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 246:1–190
Kumar PR, Bhansali A, Ravikiran M, Bhansali S, Dutta P, Thakur JS, Sachdeva N, Bhadada SK, Walia R (2010) Utility of glycated hemoglobin in diagnosing type 2 diabetes mellitus: a community-based study. J Clin Endocrinol Metab 95:2832–2835
Lee HS, Park HK, Hwang JS (2012) HbA1c and glucose intolerance in obese children and adolescents. Diabet Med 29(7):e102–e105
Libman IM, Barinas-Mitchell E, Bartucci A, Robertson R, Arslanian S (2008) Reproducibility of the oral glucose tolerance test in overweight children. J Clin Endocrinol Metab 93:4231–4237
Lippi G, Mattiuzzi C, Targher G (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362:2030 author reply 2031
Morrison KM, Xu L, Tarnopolsky M, Yusuf Z, Atkinson SA, Yusuf S (2012) Screening for dysglycemia in overweight youth presenting for weight management. Diabetes Care 35:711–716
Neu A, Feldhahn L, Ehehalt S, Hub R, Ranke MB, DIARY group Baden-Württemberg (2009) Type 2 diabetes mellitus in children and adolescents is still a rare disease in Germany: a population-based assessment of the prevalence of type 2 diabetes and MODY in patients aged 0–20 years. Pediatr Diabetes 10:468–473
Nowicka P, Santoro N, Liu H, Lartaud D, Shaw MM, Goldberg R, Guandalini C, Savoye M, Rose P, Caprio S (2011) Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 34:1306–1311
Rami B, Schober E, Nachbauer E, Waldhor T, Austrian Diabetes Incidence Study Group (2003) Type 2 diabetes mellitus is rare but not absent in children under 15 years of age in Austria. Eur J Pediatr 162:850–852
Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K, Savoye M, Rieger V, Taksali S, Barbetta G, Sherwin RS, Caprio S (2002) Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 346:802–810
Tanaka Y, Atsumi Y, Matsuoka K, Mokubo A, Asahina T, Hosokawa K, Shimada S, Matsunaga H, Takagi M, Ogawa O, Onuma T, Kawamori R (2001) Usefulness of stable HbA(1c) for supportive marker to diagnose diabetes mellitus in Japanese subjects. Diabetes Res Clin Pract 53:41–45
Tavintharan S, Chew LS, Heng DM (2000) A rational alternative for the diagnosis of diabetes mellitus in high risk individuals. Ann Acad Med Singap 29:213–218
Tsay J, Pomeranz C, Hassoun A, Zandieh SO, Rutledge J, Vogiatzi MG, Oberfield SE, Motaghedi R (2010) Screening markers of impaired glucose tolerance in the obese pediatric population. Horm Res Paediatr 73:102–107
Weiss R, Taksali SE, Tamborlane WV, Burgert TS, Savoye M, Caprio S (2005) Predictors of changes in glucose tolerance status in obese youth. Diabetes Care 28:902–909
Wiegand S, Maikowski U, Blankenstein O, Biebermann H, Tarnow P, Grüters A (2004) Type 2 diabetes and impaired glucose tolerance in European children and adolescents with obesity—a problem that is no longer restricted to minority groups. Eur J Endocrinol 151:199–206
Zeitler P, J F, Tandon N, Nadeau K, Urakami T, Barrett T, Maahs D, International Society for Pediatric and Adolescent Diabetes (2014) ISPAD Clinical Practice Consensus Guidelines 2014. Type 2 diabetes in the child and adolescent. Pediatr Diabetes 15(Suppl. 20):26–46
Ziemer DC, Kolm P, Weintraub WS, Vaccarino V, Rhee MK, Twombly JG, Narayan KM, Koch DD, Phillips LS (2010) Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med 152:770–777
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.”
Conflict of interest
The authors declare that they have no competing interests.
Funding
W.K., T.R., M.W., and S.W. were supported by grants of the German Federal Ministry of Education and Research (BMBF) (project funding reference number 01GI1120A). This part of the study is integrated in the German Competence Network on Obesity (CNO). S.W. was supported by German Research Foundation (DFG), project “Hormonal regulation of body weight maintenance” (KFO 218). G. Bi., S.E., A.N., and M.B.R. were supported by a research grant from the Tübingen University Hospital (AKF-Program, nr. 221-2-0). A.K. was supported by German Research Foundation (DFG) for the Clinical Research Center “Obesity Mechanisms” CRC1052/1 C05 and the Integrated Research and Treatment Centre (IFB) Adiposity Diseases FKZ: 01EO1001.
Additional information
Communicated by Beat Steinmann
S.E., S.W., and A.K. contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ehehalt, S., Wiegand, S., Körner, A. et al. Diabetes screening in overweight and obese children and adolescents: choosing the right test. Eur J Pediatr 176, 89–97 (2017). https://doi.org/10.1007/s00431-016-2807-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2807-6