Abstract
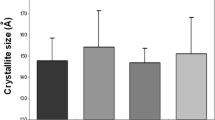
Individuals with type 2 diabetes (T2D) have a higher fracture risk compared to non-diabetics, even though their areal bone mineral density is normal to high. Identifying the mechanisms whereby diabetes lowers fracture resistance requires well-characterized rodent models of diabetic bone disease. Toward that end, we hypothesized that bone toughness, more so than bone strength, decreases with the duration of diabetes in ZDSD rats. Bones were harvested from male CD(SD) control rats and male ZDSD rats at 16 weeks (before the onset of hyperglycemia), at 22 weeks (5–6 weeks of hyperglycemia), and at 29 weeks (12–13 weeks of hyperglycemia). There were at least 12 rats per strain per age group. At 16 weeks, there was no difference in either body weight or glucose levels between the two rat groups. Within 2 weeks of switching all rats to a diet with 48 % of kcal from fat, only the ZDSD rats developed hyperglycemia (>250 mg/dL). They also began to lose body weight at 21 weeks. CD(SD) rats remained normoglycemic (<110 mg/dL) on the high-fat diet and became obese (>600 g). From micro-computed tomography (μCT) analysis of a lumbar vertebra and distal femur, trabecular bone volume did not vary with age among the non-diabetic rats but was lower at 29 weeks than at 16 weeks or at 22 weeks for the diabetic rats. Consistent with that finding, μCT-derived intra-cortical porosity (femur diaphysis) was higher for ZDSD following ~12 weeks of hyperglycemia than for age-matched CD(SD) rats. Despite an age-related increase in mineralization in both rat strains (μCT and Raman spectroscopy), material strength of cortical bone (from three-point bending tests) increased with age only in the non-diabetic CD(SD) rats. Moreover, two other material properties, toughness (radius) and fracture toughness (femur), significantly decreased with the duration of T2D in ZDSD rats. This was accompanied by the increase in the levels of the pentosidine (femur). However, pentosidine was not significantly higher in diabetic than in non-diabetic bone at any time point. The ZDSD rat, which has normal leptin signaling and becomes diabetic after skeletal maturity, provides a pre-clinical model of diabetic bone disease, but a decrease in body weight during prolonged diabetes and certain strain-related differences before the onset of hyperglycemia should be taken into consideration when interpreting diabetes-related differences.





Similar content being viewed by others
Abbreviations
- AGEs:
-
Advanced glycation end products
- α-ABA:
-
Alpha-amino-N-butyric acid
- aBMD:
-
Areal bone mineral density
- Ct.Ar:
-
Bone cross-sectional area
- BW:
-
Body weight
- BV/TV:
-
Bone volume fraction
- CD(SD):
-
CD IGS rat (Clr:CD(SD)) from Charles River
- Conn.D:
-
Connectivity density
- Ct.Th:
-
Cortical thickness
- Ct.TMD:
-
Cortical tissue mineral density
- K c,int :
-
Crack initiation toughness
- DPD:
-
Deoxypyridinoline
- DFM:
-
Distal femur metaphysis
- C min :
-
Distance between centroid and periosteal surface
- EDTA:
-
Ethylenediaminetetraacetic acid
- HFBA:
-
Heptafluorobutyric acid
- HFD:
-
High-fat diet
- HPLC:
-
High-performance liquid chromatography
- HR-pQCT:
-
High-resolution peripheral quantitative computed tomography
- HA:
-
Hydroxyapatite
- Ct.Po:
-
Intra-cortical porosity
- μCT:
-
Micro-computed tomography
- MMR:
-
Mineral-to-matrix ratio
- I min :
-
Moment of inertia
- NEGs:
-
Non-enzymatic, glycation mediated crosslinks
- M p :
-
Peak moment
- PE:
-
Pentosidine
- PITC:
-
Phenylisothiocyanate
- PBS:
-
Phosphate buffer saline
- Po.N:
-
Pore number
- PYdisp :
-
Post-yield displacement
- PYD:
-
Pyridinoline
- PYR:
-
Pyridoxine
- RS:
-
Raman spectroscopy
- ROI:
-
Region of interest
- L:
-
Span
- 3pt:
-
Three-point bending
- Tt.Ar:
-
Total cross-sectional area
- Tb.N:
-
Trabecular number
- Tb.Th:
-
Trabecular thickness
- Tb.TMD:
-
Trabecular tissue mineral density
- T2D:
-
Type 2 diabetes
- VB:
-
Vertebral body
- W f :
-
Work-to-fracture
- ZDF:
-
Zucker diabetic fatty
- ZDSD:
-
Zucker diabetic Sprague–Dawley from PreClinOmics
References
Bonds DE, Larson JC, Schwartz AV, Strotmeyer JR, Rodriguez BL, Johnson KC, Margolis KL (2006) Risk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational Study. J Clin Endocrinol Metab 91:3404–3410
Vestergaard P, Rejnmark L, Mosekilde L (2009) Diabetes and its complications and their relationship with risk of fractures in type 1 and 2 diabetes. Calcif Tissue Int 84:45–55
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Seeley DG (1996) Predictors of ankle and foot fractures in older women. J Bone Miner Res 11:1347
de Liefde II, van der Klift M, de Lae CE, van Daele PL, Hofman A, Pols HA (2005) Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam study. Osteoporos Int 16:1713–1720
Leslie WD, Lix LM, Prior HJ, Derksen S, Metge C, O’Neil J (2007) Biphasic fracture risk in diabetes: a population-based study. Bone 40:1595–1601
Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE et al (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305:2184–2192
Burghardt A, Issever AS, Schwartz AV, Davis KA, Masharani U, Majumdar S et al (2010) High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 95:5045–5055
Farr JN, Drake MT, Amin S, Melotn LJ 3rd, McCready LK, Khosla S (2014) In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res 29:787–795
Yu E, Putman MS, Derrico N, Abrishamanian-Garcia G, Finkelstein JS, Bouxsein ML (2015) Defects in cortical microarchitecture among African-American women with type 2 diabetes. Osteoporos Int 26:673–679
Patsch JM, Burghardt AJ, Yap SP, Baum T, Schwartz AV, Joseph GB, Link TM (2013) Increased cortical porosity in type 2 diabetic postmenopausal women with fragility fractures. J Bone Miner Res 28:313–324
Heilmeier U, Carpenter DR, Patsch JM, Harnish R, Joseph GB, Burghardt AJ, Baum T, Schwartz AV, Lang TF, Link TM (2015) Volumetric femoral BMD, bone geometry, and serum sclerostin levels differ between type 2 diabetic postmenopausal women with and without fragility fractures. Osteoporos Int 26:1283–1293
Vestergaard P (2006) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes: a meta-analysis. Osteoporos Int 18:427–444
Nyman JS, Roy A, Tyler JH, Acuna RL, Gayle HJ, Wang X (2007) Age-related factors affecting the postyield energy dissipation of human cortical bone. J Orthop Res 25:646–655
Karim L, Tang SY, Sroga GE, Vashishth D (2013) Differences in non-enzymatic glycation and collagen cross-links between human cortical and cancellous bone. Osteoporos Int 24:2441–2447
Zimmermann EA, Schaible E, Bale H, Barth HD, Tang SY, Reichert P, Busse B, Alliston T, Ager JW 3rd, Ritchie RO (2011) Age-related changes in the plasticity and toughness of human cortical bone at multiple length scales. Proc Natl Acad Sci USA 108:14416–144421
Monnier V, Sun W, Sell DR, Fan X, Nemet I, Genuth S (2014) Glucosepane: a poorly understood advanced glycation end product of growing importance for diabetes and its complications. Clin Chem Lab Med 52:21–32
Oren TW, Botolin S, Williams A, Buckness A, King KB (2011) Arthroplasty in veterans: analysis of cartilage, bone, serum, and synovial fluid reveals differences and similarities in osteoarthritis with and without comorbid diabetes. J Rehabil Res Dev 48:1195–1210
Saito M, Kida Y, Kato S, Marumo K (2014) Diabetes, collagen and bone quality. Curr Osteoporos Rep 12:181–188
Hill Gallant KM, Gallant MA, Brown DM, Sato AY, Williams JN, Burr DB (2014) Raloxifene prevents skeletal fragility in adult female Zucker Diabetic Sprague-Dawley rats. PLoS One 9:e108262
Prisby RD, Swift JM, Bloomfield SA, Hogan HA, Delp MD (2008) Altered bone mass, geometry, and mechanical properties during the development and progression of type 2 diabetes in the Zucker diabetic fatty rat. J Endocrinol 199:379–388
Hamann C, Picke AK, Campbell GM, Balyura M, Rauner M, Bernhardt R, Huber G, Morlock MM, Günther KP, Borstein Stefan R, Gluer Claus-C, Ludwig Barbara, Hofbauer Lorenz C (2014) Effects of parathyroid hormone on bone mass, bone strength, and bone regeneration in male rats with type 2 diabetes mellitus. Endocrinology 155:1197
Reinwald S, Peterson RG, Allen MR, Burr DB (2009) Skeletal changes associated with the onset of type 2 diabetes in the ZDF and ZDSD rodent models. Am J Physiol Endocrinol Metab 296:E765–E774
Nyman JS (2013) Effect of diabetes on the fracture resistance of bone. Clinic Rev Bone Miner Metab 11:38–48
Fajardo RJ, Karim L, Calley VI, Bouxsein ML (2014) A review of rodent models of type 2 diabetic skeletal fragility. J Bone Miner Res 29:1025–1040
Hammond MA, Gallant MA, Burr DB, Wallace JM (2014) Nanoscale changes in collagen are reflected in physical and mechanical properties of bone at the microscale in diabetic rats. Bone 60:26–32
Peterson RG, Jackson CV, Zimmerman K, de Winter W, Hueber N, Hansen MK (2015) Characterization of the ZDSD rat: a translational model for the study of the metabolic syndrome and type 2 diabetes. J Diabetes Res. Article ID 487816
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25:1468–1486
Uppuganti S, Granke M, Makowski AJ, Does MD, Nyman JS (2016) Age-related changes in the fracture resistance of male Fischer F344 rat. Bone 83:220–232
Silva MJ, Brodt MD, Lynch MA, McKenzie JA, Tanouye KM, Nyman JS, Wang X (2009) Type 1 diabetes in young rats leads to progressive trabecular bone loss, cessation of cortical bone growth, and diminished whole bone strength and fatigue life. J Bone Miner Res 24:1618–1627
Ritchie R, Koester KJ, Ionova S, Yao W, Lane NE, Ager JW (2008) Measurement of the toughness of bone: a tutorial with special reference to small animals. Bone 43:798–812
Makowski AJ, Uppuganti S, Wadeer SA, Whitehead JM, Rowland BJ, Granke M, Mahadevan-Jansen A, Yang X, Nyman JS (2014) The loss of activating transcription factor 4 (ATF4) reduces bone toughness and fracture toughness. Bone 62:1–9
Makowski AJ, Pence IJ, Uppuganti S, Zein-Sabatto A, Huszagh MC, Mahadevan-Jansen A, Nyman JS (2014) Polarization in Raman spectroscopy helps explain bone brittleness in genetic mouse models. J Biomed Opt 19:117008
Buckley A, Hill KE, Davidson JS (1988) Collagen metabolism. In: Di Sabato G, Abelson J, Simon M (eds) Methods in enzymology. Academic Press, San Diego, pp 674–694
Shanbhogue V, Michell DM, Rosen CJ, Bouxsein ML (2015) Type 2 diabetes and the skeleton: new insights into sweet bones. Lancet Diabetes Endocrinol 4:159–173
Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, Armstrong D, Ducy P, Karsenty G (2002) Leptin regulates bone formation via the sympathetic nervous system. Cell 111:305–317
Shi Y, Yadav VK, Suda N, Liu XS, Guo XE, Myers MG, Karsenty G (2008) Dissociation of the neuronal regulation of bone mass and energy metabolism by leptin in vivo. Proc Natl Acad Sci USA 105:20529–20533
Davidson E, Coppey, LJ, Holmes A, Lupachy S, Dake BL, Oltman CL, Peterson RG, Yorek MA (2014) Characterization of diabetic neuropathy in the Zucker Diabetic Sprague-Dawley Rat: a new animal model for type 2 diabetes. J Diabetes Res. Article ID 714273
Gallant MA, Brown DM, Organ JM, Allen MR, Burr DB (2013) Reference-point indentation correlates with bone toughness assessed using whole-bone traditional mechanical testing. Bone 53:301–305
Saito M, Fujii K, Mori Y, Marumo K (2006) Role of collagen enzymatic and glycation induced cross-links as a determinant of bone quality in spontaneously diabetic WBN/Kob rats. Osteoporos Int 17:1514–1523
Makowski A, Patil CA, Mahadevan-Jansen A, Nyman JS (2013) Polarization control of Raman spectroscopy optimizes the assessment of bone tissue. J Biomed Opt 18:55005
Acknowledgments
The Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development (1I01BX001018) primarily funded the present work. The fund for the purchase of the micro-computed tomography scanner was provided by the National Center for Research Resources (1S10RR027631) and matching funds from the Vanderbilt Office of Research. There was additional support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (NIH grants AR063157 and 1T32DK101003) and the National Science Foundation (1068988). The Vanderbilt Hormone Assay and Analytical Services Core is supported by NIH grants DK059637 and DK020593. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Amy Creecy, Sasidhar Uppuganti, Alyssa R. Merkel, Dianne O’Neal, Alexander J. Makowski, Mathilde Granke, Paul Voziyan, and Jeffry S. Nyman have declared no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Creecy, A., Uppuganti, S., Merkel, A.R. et al. Changes in the Fracture Resistance of Bone with the Progression of Type 2 Diabetes in the ZDSD Rat. Calcif Tissue Int 99, 289–301 (2016). https://doi.org/10.1007/s00223-016-0149-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-016-0149-z