Abstract
Aims/hypothesis
Glucose fluctuations may help predict diabetic complications. We evaluated the relation between glucose variability and oxidative stress in patients with type 1 diabetes.
Methods
Continuous glucose monitors were inserted subcutaneously in 25 patients. During the measurement, patients collected two 24 h urine samples, while 24 healthy controls collected one 24 h urine sample for determination of 15(S)-8-iso-prostaglandin \( {\text{F}}_{{2\alpha }} {\left( {{\text{PGF}}_{{2\alpha }} } \right)} \) using HPLC tandem mass spectrometry. Mean of the daily differences (MODD), mean amplitude of glycaemic excursions (MAGE) and continuous overlapping net glycaemic action calculated with n hour time-intervals (CONGA-n) were calculated as markers for glucose variability and correlation with \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion was calculated.
Results
Median [interquartile range (IQR)] urinary \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) was higher in patients than healthy controls: 161 (140–217) pg/mg creatinine vs 118 (101–146) pg/mg creatinine (p = 0.001). Median (IQR) MODD was 3.7 (3.2–5.0) mmol/l, MAGE 7.6 (6.4–9.0) mmol/l and CONGA-1 2.3 (2.1–2.8) mmol/l. Univariate regression did not reveal an association for MODD (r 2 = 0.01), MAGE (0.08) or CONGA-1 (0.07) with \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion, nor was an association revealed when corrected for HbA1c, age, sex and smoking. Spearman correlation coefficients (r) between \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion and MODD, MAGE and CONGA-1 were non-significant: −0.112, −0.381 and −0.177.
Conclusions/interpretation
We report that there is no relationship between glucose variability and urinary \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \). We also confirm that patients with type 1 diabetes have higher levels of urinary \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) than healthy controls, suggesting that in addition to glucose variability, other factors favouring oxidative stress may exist. We did not see a relation between high glucose variability and elevated levels of oxidative stress in patients with type 1 diabetes.
Similar content being viewed by others
Introduction
Hyperglycaemia is the main risk factor for developing microvascular complications and accelerates atherosclerosis in diabetes [1, 2]. The present paradigm postulates that mitochondrial glucose overload results in increased electron transfer to oxygen and formation of free oxygen radicals. This in turn activates four pathways along which hyperglycaemia can induce diabetic complications [3]. There is also some evidence that hypoglycaemia may contribute to platelet activation and thereby to macrovascular complications. The mechanisms through which both hyper- and hypoglycaemia contribute to diabetic complications is schematically depicted in Fig. 1 [4, 5].
Recent studies with continuous glucose sensors found a large range of glucose values in children with type 1 diabetes, even in those with excellent HbA1c values, which raises the possibility that in addition to HbA1c, glucose variability may have predictive value for the development of diabetic complications [6–8]. Although this has been negated for microvascular complications [9], it is an attractive hypothesis to explain the increased macrovascular burden of type 1 diabetes [10]. A recent study investigated the effect of long-term glycaemic exposure, as indicated by HbA1c, and acute glucose fluctuations quantified with a continuous glucose monitor on the activation of oxidative stress in 21 type 2 diabetic patients on either oral glucose-lowering medication or a weight-controlling diet and compared activation of oxidative stress with age and sex-matched healthy control persons. This study revealed significantly more oxidative stress in patients with type 2 diabetes than in healthy control persons and demonstrated that acute glucose fluctuations in particular induce oxidative stress. These fluctuations were suggested to be valuable predictors for the risk of diabetic complications [11]. Activation of oxidative stress was estimated from the measurement of 24 h urinary excretion of 8-iso-prostaglandin \( {\text{F}}_{{2\alpha }} {\left( {{\text{PGF}}_{{2\alpha }} } \right)} \). Because isoprostanes are stable products from free oxygen radical-mediated oxidation of arachidonic acid and have been demonstrated to increase with oxidant injury, they are considered good indicators of oxidative stress [12, 13]. The daily glucose fluctuations were quantified with the mean amplitude of glucose excursions (MAGE), calculated from the continuous sensor readings [11].
To date, the role of acute glucose fluctuations in activation of oxidative stress has not been investigated in patients with type 1 diabetes. Insulin therapy, higher insulin sensitivity and affected counter-regulation to hypoglycaemia will contribute to more pronounced glucose fluctuations in patients with type 1 diabetes than in those with type 2 diabetes. The aim of our study was to evaluate the role of glucose variability, assessed using a continuous glucose monitor, in the activation of oxidative stress in patients with type 1 diabetes and to determine the amount of oxidative stress in these patients as compared with healthy control persons.
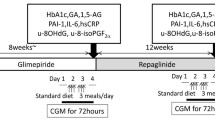
Methods
Patients
The study was approved by the local ethics committee and participants gave written informed consent. Twenty-five patients with type 1 diabetes and 24 age- and sex-matched healthy controls were enrolled in the study. The main clinical characteristics are listed in Table 1. Hypertension was defined as receiving antihypertensive treatment. Diabetic retinopathy, nephropathy and neuropathy were defined as having had laser coagulation, microalbuminuria requiring therapy with ACE inhibition and altered or diminished sensibility in hands and/or feet, respectively. Macrovascular complications were defined as coronary artery diseases, e.g. angina pectoris or acute myocardial infarction, and/or cerebrovascular events in the medical history. Seven patients were using an insulin pump, all with a rapid-acting analogue as pump insulin, and 18 patients were being treated with multiple daily injections. Of the latter, 13 were on a combination of long and rapid-acting insulin analogues (glargine, detemir and lispro, aspart), one on human insulin only, three on a combination of rapid-acting human insulin and basal insulin analogues and one on rapid-acting insulin analogues and basal human insulin.
Exclusion criteria were a BMI > 30 kg/m2, a GFR of less than 60 ml min−1 1.73 m−2 according to the Cockcroft–Gault formula [14], heparin, oral anticoagulants or corticosteroid use, skin conditions prohibiting sensor needle insertion and any febrile illnesses during the 3 month period prior to the experiment.
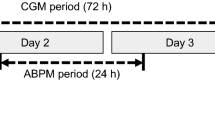
Study protocol
The experiment consisted of two short visits to the clinical trial room. During the first visit the continuous glucose sensor (CGMSgold; MedtronicMiniMed, Sylmar, CA, USA) was inserted subcutaneously in the abdominal periumbilical area of the patients and, if present, the insulin pump on the other side. Patients injecting insulin were asked not to inject on the same side as the sensor insertion side in the week prior to and during the period of measurement. Home blood glucose meters (Accu-Check Compact Plus; Roche Diagnostics, Quebec, Canada) were provided to perform the sensor calibration procedure four times daily. Information about diabetes duration, complications and current mode and dose of insulin therapy was recorded in the case record form. A venous blood sample was collected for HbA1c determination. Patients were asked to collect urine during two consecutive 24 h periods. They were instructed to preserve the urine-containing jars in the refrigerator when at home and in special cooling bags when outdoors, in order to avoid artificial formation of isoprostanes. For optimal prevention of artificial isoprostane formation, patients noted the total urine volume after 24 h, mixed the urine thoroughly, and divided 14 ml urine equally into two tubes, which were placed in a freezer until the second visit. The same procedure was done with the second 24 h urine collection. In addition, patients received a study diary to record their meals and symptomatic hypo- or hyperglycaemic events. Three days later, patients returned to hospital to have the sensor removed and data downloaded, and to hand in the frozen urine tubes together with the study diary. Healthy controls were asked to do one 24 h urine collection, as described above for the patients with type 1 diabetes. For both the patients and healthy controls, age, concomitant medication, smoking, height and weight and the resulting BMI were recorded. As the association with lower oxidative stress levels is still controversial [15–18], participants were asked not to take vitamin E tablets during the experiment. Finally, the urine-containing tubes were stored at −80°C until analyses for \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) and creatinine in one run.
Laboratory measurements
HbA1c was measured using an HPLC assay (Variant II; Bio-Rad Laboratories, Montreal, QC, Canada). Activation of oxidative stress was estimated by determining the urinary isoprostane excretion (\( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \)), using HPLC tandem mass spectrometry (HPLC-MS/MS). Urine samples were collected and stored without additives as 7 ml aliquots at −80°C. Initial creatinine concentrations were established by colorimetric Jaffé assay. Two millilitres of sample was mixed with 2H4-labelled \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) as internal standard and applied to an \( 8 - iso - {\text{PGF}}_{{2\alpha }} \) immunoaffinity column (CaymanChemical Company, Ann Arbor, MI, USA). After washing, the extract was eluted, evaporated to dryness (60°C, N2) and reconstituted in 200 μl 0.05 mol/l formic acid–ethanol (75:25, vol./vol.); 50 μl was injected on the HPLC-MS/MS. Chromatographic separation was achieved on a modular HPLC system (Surveyor; Thermo Finnigan, San Jose, CA, USA) consisting of a cooled autosampler (T = 12°C), a low-flow quaternary MS pump and analytical HPLC column: 2.1 × 150 mm, 5 μm Alltech C8 (Alltech Lexington, KT, USA). Samples were eluted with a flow rate of 200 μl/min and a programmed gradient between A (HCOOH–H2O; 0.01%, vol./vol.) and B (CH3CN). MS/MS analyses were performed on a TSQ Quantum AM (Thermo Finnigan) operated in the positive ion electrospray ionisation mode. The surface-induced dissociation was set at 15 V; spray voltage was 3,000 V and the capillary temperature was 300°C. In the MS/MS experiments argon was used as collision gas at a pressure of 0.2 Pa; collision energy was 20 eV for the optimised transitions: m/z 353.24→m/z 193 and m/z 357.24→m/z 197.10. The inter-assay (n = 5) and intra-assay (average of 5 days, n = 3) variability allowed for determination at physiological concentrations with a CV < 7%.
Assessment of glycaemic variability
Inter-day glycaemic variability
The day-to-day variation of the glucose pattern was calculated with the mean of the daily differences (MODD), which is defined as the mean of the absolute differences between glucose values on day 2 and the corresponding values on day 1, at the same time [19, 20].
Intra-day glycaemic variability
Because there is no consensus on how to optimally assess glucose variability and to prevent the results from being affected by the method chosen, we performed multiple calculations to estimate the glucose variability. The easiest measure is the CV defined as the SD divided by the mean of the glucose values. Another marker of glucose variability is the MAGE, designed by Service et al. [21] in 1970. The MAGE over 24 h is the mean of the absolute differences between peak and nadir values over 24 h, with peaks (nadirs) defined as glucose values preceded and followed by an increase (decrease) and decrease (increase), respectively, in excess of at least 1 SD of the mean glucose. If a decrease of more than 1 SD was the first excursion, only peak-to-nadir excursions (>1 SD) were included in the calculation of the MAGE and vice versa. We calculated the MAGE over both 24 h urine collection periods separately and over the two periods taken together.
Rapid glucose variability
We also calculated the recently proposed continuous overlapping net glycaemic action calculated with n hour time-intervals (CONGA-n), to gain insight into the rapid glucose variability. With this method, the difference between each glucose reading and the glucose reading n hours previously (as determined by the investigator) is calculated. The CONGA-n is the standard deviation of these differences. We used CONGA-1, indicating intra-day variability based on 1 h time differences, to allow for comparison of our results with those reported in other articles [19, 22]. In normal non-diabetic participants, CONGA values vary between 0.4 and 1.2: values above 1.5 indicate glycaemic lability [19]. Furthermore, we calculated the within-hour glucose SD and range, as markers of rapid glucose variability.
Statistical analysis
Mean urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), inter- and intra-day and rapid glucose variability were assessed using standard statistics. The intra-individual day-to-day variation of the above-mentioned variables was calculated using a paired samples t test or Wilcoxon’s signed rank test, depending on the distribution of the data. Oxidative stress was compared between the patients with type 1 diabetes and the age and sex-matched healthy controls, using an independent samples t test or Mann–Whitney U test, again depending on the distribution of the data. Correlation was calculated and univariate regression analysis was performed to evaluate the relation between the excretion rate of urinary \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) and the markers of glycaemic variability, results being corrected in multivariate regression analysis for long-term glycaemic control as indicated by the HbA1c level [15, 23], sex [24], age [25] and smoking [17, 18, 26], all variables that have been reported to be involved in the activation of oxidative stress. For lipid values and blood pressure, we also evaluated the association with urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) in a univariate model. In the event of a significant relation in the univariate analysis, variables were included in a multivariate model to evaluate the determinants for oxidative stress. p values of <0.05 were considered significant.
Results
One patient discontinued the sensor measurement after approximately 24 h, because of a putative allergic reaction against the inserted sensor needle. Patients wore the continuous glucose monitor for a period ranging from 50 to 72 h. In total, data of continuous glucose measurements during 49 24-h periods, together with the concomitant urinary \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion levels, were obtained in 25 patients with type 1 diabetes. The \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion levels during a single 24-h period were obtained in 24 age- and sex-matched healthy controls. There were no major differences in age, BMI and smoking between the two groups (see Table 1).
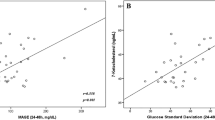
Data on inter-day, intra-day and rapid glycaemic variability are summarised in Table 2. The median (interquartile range [IQR]) urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), calculated over two urine collection periods, in the patient group was 161 (140–217) pg/mg creatinine (Fig. 2). There was no significant difference in \( 8 - iso - {\text{PGF}}_{{2\alpha }} \) excretion between the first and the second urine collection (172 [147–231] pg/mg creatinine vs 157 [139–218] pg/mg creatinine, p = 0.162, Wilcoxon signed rank test), while the between-patient variability significantly exceeded the within-patient variability (p = 0.009, Kruskal–Wallis test). The median (IQR) urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) was significantly lower in healthy control persons than in diabetes patients: 118 (101–146) pg/mg creatinine (p = 0.001, Mann–Whitney U test). Data on MAGE and oxidative stress, assessed in the patients with type 1 diabetes, are plotted in Fig. 3, clearly illustrating the absence of any relationship between these two variables. Univariate regression analysis revealed that none of the markers of glucose variability were associated with the urinary excretion rate of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) (analysed as dependent variable, with maximum r 2 values of 0.01, 0.08 and 0.07 for the inter-day, intra-day and rapid glucose variability, respectively). In addition, no significant relationship was found between blood pressure, hypertension and lipid values (HDL-cholesterol, total cholesterol, triacylglycerol) on the one hand, and the amount, on the other hand, of oxidative stress, as can be seen from poor r 2 values ranging from 0.002 (p = 0.85) for triacylglycerol values to 0.056 (p = 0.364) for systolic blood pressure. Correction for HbA1c, sex, age and smoking did not reveal a significant association for any of the markers. Regression analysis, with and without correction for HbA1c, age and smoking, revealed that sex had the strongest, though very poor, association with oxidative stress (r 2 = 0.1, p = 0.085). Regression analysis over the total study group, including patients and control persons, revealed that smoking, but not sex and age, had a significant though weak association (r 2 = 0.14, p = 0.036) with oxidative stress.
Correlations between \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) and the markers of glucose variability are given in Table 3. Again, none of the markers of glucose variability were associated with the urinary excretion rate of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \).
Discussion
In this study, none of the measures of glucose variability was associated with oxidative stress, estimated by the urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), in patients with type 1 diabetes. In accordance with previously reported studies, our results confirm that patients with type 1 diabetes have higher levels of oxidative stress than healthy controls matched for age and sex [15, 23, 27, 28].
Because MAGE depends on the frequency of glucose measurements and the direction, either peak-to-nadir or nadir-to-peak, of the glucose excursions [21], it is open to several interpretations and is not acknowledged as the gold standard for glucose variability. So, to account for the influence of the method chosen, we calculated various different markers for glucose variability. The mean MODD and CONGA-1 for the 25 patients in our study appeared to be similar to values reported for ten patients with type 1 diabetes in an earlier study [19] (MODD, 4.0 mmol/l vs 4.3 mmol/l and CONGA-1, 2.5 mmol/l, in that and our studies). The mean MAGE in our study was higher than previously reported for 21 patients with type 2 diabetes (8.3 vs 4.2 mmol/l) [11], confirming that glucose variability in patients with type 1 diabetes is higher than in those with type 2 diabetes. Thus, based on the higher MAGE and the correlation reported earlier between glucose variability and the activation of oxidative stress, we expected a strong association between the excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) and glucose variability in our study group [11]. Our failure to find a relationship between glucose variability and oxidative stress contrasts sharply with the strong correlation (r = 0.86) between MAGE and urinary excretion of \( 8 - iso - {\text{PGF}}_{{2\alpha }} \), as previously reported for patients with type 2 diabetes [11]. With MAGE as the only reported marker of glucose variability, that study of patients with type 2 diabetes does not allow a complete comparison with respect to glucose variability measures in relation to oxidative stress.
According to our data, HbA1c, sex, age and smoking were not related to oxidative stress. The role of these factors in the activation of oxidative stress is being debated, given the fact that other studies were either unable to detect an association for HbA1c [29] and age [24, 26] with oxidative stress or reported conflicting data on the effect of sex, with both male [30, 31] and female [24] sex being associated with increased activation of oxidative stress. The limited number of smokers might explain why our results on smoking are not in accordance with earlier reports on the association between smoking and elevated urinary excretion of 8-isoprostanes [17, 18, 26].
An explanation for the lack of correlation between glucose variability and oxidative stress may be that, unlike patients with type 2 diabetes, patients with type 1 diabetes are not sensitive to glucose variability as a stimulator of oxidative stress, because of different underlying pathophysiological mechanisms [28, 32–35]. The significantly higher excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) in patients with type 1 diabetes as compared with healthy controls does suggest the existence of a factor favouring oxidative stress. However, glucose variability, despite being greater than in type 2 diabetes, does not seem to be this factor.
At first glance, the excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) in patients and healthy control persons was substantially lower in our study than in several previous studies [11, 15]. Rather than an immunoassay, we used tandem mass spectrometry, a modern and precise method, which is not sensitive to components other than 8-isoprostanes. This sensitivity has been acknowledged to be a possible confounding factor when using an immunoassay [11]. The method used in our study selectively determined \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), while less specific methods include its enantiomere ent-\( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) in the quantification of oxidative stress. This is why in the literature \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \) levels are often reported to be higher.
In conclusion, we report that there is no relationship between urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), determined with a highly specific method, and various measures of glucose variability. Our findings confirm that the amount of oxidative stress, estimated by urinary excretion of \( 15{\left( S \right)} - 8 - iso - {\text{PGF}}_{{2\alpha }} \), is higher in patients with type 1 diabetes than in healthy control persons, arguing against a role of glucose variability in the activation of oxidative stress.
Abbreviations
- CONGA-n :
-
continuous overlapping net glycaemic action calculated with n hour time-intervals
- HPLC MS/MS:
-
HPLC tandem mass spectrometry
- IQR:
-
interquartile range
- MAGE:
-
mean amplitude of glycaemic excursions
- MODD:
-
mean of the daily differences
- \( {\text{PGF}}_{{2\alpha }} \) :
-
prostaglandin \( {\text{F}}_{{2\alpha }} \)
References
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
Evans M (1998) The UK prospective diabetes study. Lancet 352:1932–1933
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625
Monnier LH, Lachkar H, Richard JL et al (1984) Plasma beta-thromboglobulin response to insulin-induced hypoglycemia in type I diabetic patients. Diabetes 33:907–909
Trovati M, Anfossi G, Cavalot F et al (1986) Studies on mechanisms involved in hypoglycemia-induced platelet activation. Diabetes 35:818–825
Boland E, Monsod T, Delucia M, Brandt CA, Fernando S, Tamborlane WV (2001) Limitations of conventional methods of self-monitoring of blood glucose: lessons learned from 3 days of continuous glucose sensing in pediatric patients with type 1 diabetes. Diabetes Care 24:1858–1862
Ceriello A, Motz E (2004) Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 24:816–823
Salardi S, Zucchini S, Santoni R et al (2002) The glucose area under the profiles obtained with continuous glucose monitoring system relationships with HbA(lc) in pediatric type 1 diabetic patients. Diabetes Care 25:1840–1844
Kilpatrick ES, Rigby AS, Atkin SL (2006) The effect of glucose variability on the risk of microvascular complications in type 1 diabetes. Diabetes Care 29:1486–1490
Nathan DM, Cleary PA, Backlund JY et al (2005) Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 353:2643–2653
Monnier L, Mas E, Ginet C et al (2006) Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295:1681–1687
Morrow JD, Hill KE, Burk RF, Nammour TM, Badr KF, Roberts LJ (1990) A series of prostaglandin F2-like compounds are produced in vivo in humans by a non-cyclooxygenase, free radical-catalyzed mechanism. Proc Natl Acad Sci U S A 87:9383–9387
Roberts LJ, Morrow JD (2000) Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic Biol Med 28:505–513
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Davi G, Ciabattoni G, Consoli A et al (1999) In vivo formation of 8-iso-prostaglandin f2alpha and platelet activation in diabetes mellitus: effects of improved metabolic control and vitamin E supplementation. Circulation 99:224–229
Meagher EA, Barry OP, Lawson JA, Rokach J, Fitzgerald GA (2001) Effects of vitamin E on lipid peroxidation in healthy persons. JAMA 285:1178–1182
Patrignani P, Panara MR, Tacconelli S et al (2000) Effects of vitamin E supplementation on F(2)-isoprostane and thromboxane biosynthesis in healthy cigarette smokers. Circulation 102:539–545
Reilly M, Delanty N, Lawson JA, Fitzgerald GA (1996) Modulation of oxidant stress in vivo in chronic cigarette smokers. Circulation 94:19–25
McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron FJ (2005) A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther 7:253–263
Molnar GD, Taylor WF, Ho MM (1972) Day-to-day variation of continuously monitored glycaemia: a further measure of diabetic instability. Diabetologia 8:342–348
Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood LC, Taylor WF (1970) Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes 19:644–655
Praet SF, Manders RJ, Meex RC et al (2006) Glycaemic instability is an underestimated problem in Type II diabetes. Clin Sci (Lond) 111:119–126
Flores L, Rodela S, Abian J, Claria J, Esmatjes E (2004) F2 isoprostane is already increased at the onset of type 1 diabetes mellitus: effect of glycemic control. Metabolism 53:1118–1120
Block G, Dietrich M, Norkus EP et al (2002) Factors associated with oxidative stress in human populations. Am J Epidemiol 156:274–285
Wang Z, Ciabattoni G, Creminon C et al (1995) Immunological characterization of urinary 8-epi-prostaglandin F2 alpha excretion in man. J Pharmacol Exp Ther 275:94–100
Morrow JD, Frei B, Longmire AW et al (1995) Increase in circulating products of lipid peroxidation (F2-isoprostanes) in smokers. Smoking as a cause of oxidative damage. N Engl J Med 332:1198–1203
Catella-Lawson F, Fitzgerald GA (1996) Oxidative stress and platelet activation in diabetes mellitus. Diabetes Res Clin Pract 30(Suppl):13–18
Chisolm GM, Irwin KC, Penn MS (1992) Lipoprotein oxidation and lipoprotein-induced cell injury in diabetes. Diabetes 41(Suppl 2):61–66
Gopaul NK, Anggard EE, Mallet AI, Betteridge DJ, Wolff SP, Nourooz-Zadeh J (1995) Plasma 8-epi-PGF2 alpha levels are elevated in individuals with non-insulin dependent diabetes mellitus. FEBS Lett 368:225–229
Ide T, Tsutsui H, Ohashi N et al (2002) Greater oxidative stress in healthy young men compared with premenopausal women. Arterioscler Thromb Vasc Biol 22:438–442
Veglia F, Cighetti G, De FM et al (2006) Age- and gender-related oxidative status determined in healthy subjects by means of OXY-SCORE, a potential new comprehensive index. Biomarkers 11:562–573
Maxwell S, Holm G, Bondjers G, Wiklund O (1997) Comparison of antioxidant activity in lipoprotein fractions from insulin-dependent diabetics and healthy controls. Atherosclerosis 129:89–96
Maxwell SR, Thomason H, Sandler D et al (1997) Antioxidant status in patients with uncomplicated insulin-dependent and non-insulin-dependent diabetes mellitus. Eur J Clin Invest 27:484–490
Santini SA, Marra G, Giardina B et al (1997) Defective plasma antioxidant defenses and enhanced susceptibility to lipid peroxidation in uncomplicated IDDM. Diabetes 46:1853–1858
Tsai EC, Hirsch IB, Brunzell JD, Chait A (1994) Reduced plasma peroxyl radical trapping capacity and increased susceptibility of LDL to oxidation in poorly controlled IDDM. Diabetes 43:1010–1014
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript. The sensors were made available free of charge by Medtronic NL (Heerlen, the Netherlands).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wentholt, I.M.E., Kulik, W., Michels, R.P.J. et al. Glucose fluctuations and activation of oxidative stress in patients with type 1 diabetes. Diabetologia 51, 183–190 (2008). https://doi.org/10.1007/s00125-007-0842-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0842-6