Abstract
Aims/hypothesis
The pathogenesis of vascular complications in type 1 diabetes is poorly understood, but may involve chronic, low-grade inflammation. We investigated the association of markers of inflammation with vascular complications in type 1 diabetes.
Methods
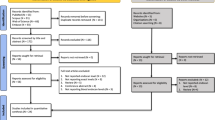
A cross-sectional nested case-control study of the follow-up data of the EURODIAB Prospective Complications Study. This study included 543 individuals (278 men) with type 1 diabetes diagnosed at <36 years of age. Cases (n=348) had complications of diabetes, controls (n=195) had no complications.
Results
C-reactive protein, interleukin-6 and tumour necrosis factor-α levels, which were combined in an inflammatory marker Z-score, were associated with albuminuria, retinopathy and cardiovascular disease. Calculated means (95% confidence intervals) of the marker Z-score were −0.15 (−0.22 to −0.07), 0.10 (−0.05 to 0.25), and 0.28 (0.15 to 0.41), p for trend <0.0001, in individuals with normo-, micro- and macroalbuminuria; −0.23 (−0.33 to −0.13), 0.14 (0.02 to 0.25) and 0.20 (0.07 to 0.32), p for trend <0.0001, in individuals with no, non-proliferative and proliferative retinopathy; and −0.28 (−0.39 to −0.18) and 0.06 (−0.08 to 0.20), p<0.001, in individuals without and with cardiovascular disease. Per 1 SD increase of the inflammatory marker Z-score, GFR decreased by −4.6 (−6.6 to −2.6) ml per min per 1.73 m2 (p<0.001).
Conclusions/interpretation
We have shown that markers of inflammation are strongly and independently associated with microvascular complications and cardiovascular disease in type 1 diabetes. These data suggest that strategies to decrease inflammatory activity may help to prevent the development of vascular complications in type 1 diabetes.
Similar content being viewed by others
The pathogenesis of vascular complications in type 1 diabetes is poorly understood. Glycaemic control and systolic blood pressure are important determinants in type 1 diabetes [1, 2], but cannot in themselves wholly account for disease occurrence.
Recent data on the pathogenesis of atherothrombosis and of (micro)albuminuria in non-diabetic and type 2 diabetic individuals have shown that inflammation plays an important role in their development [3]. As in type 2 diabetes, inflammatory activity is increased in type 1 diabetes [4]. We therefore hypothesised that inflammatory activity may be involved in the development of vascular complications in type 1 diabetes, both directly and by mediating, in part, the effects of conventional risk factors such as blood pressure, HbA1c and advanced glycation endproducts (AGEs) [5].
To test this hypothesis, we investigated the associations of markers of inflammation, i.e., C-reactive protein (CRP), interleukin-6 (IL-6), tumour necrosis factor-α (TNF-α), with the presence of microvascular complications and cardiovascular disease in type 1 diabetic patients of the EURODIAB Prospective Complications Study. In addition, we investigated whether the associations of HbA1c, the AGEs pentosidine, \({\text{N}}^{\varepsilon } \)-(carboxymethyl)lysine (CML) and \({\text{N}}^{\varepsilon } \)-(carboxyethyl)lysine (CEL), systolic blood pressure and other vascular risk factors on the one hand with microvascular complications and cardiovascular disease on the other were mediated through inflammatory activity.
Methods
Subjects
The EURODIAB Prospective Complications Study is a follow-up of the EURODIAB IDDM Complications study [6]. Baseline investigations (1988–1991) were performed on 3,250 men and women with type 1 diabetes drawn from 31 European centres. All subjects gave informed consent and the study was approved by local ethics committees. Sample selection was stratified by sex, age group and duration of diabetes, to ensure sufficient representation in all categories. Type 1 diabetes was clinically defined as a diagnosis made before the age of 36 years, with a continuous need for insulin therapy within 1 year of diagnosis. The follow-up was performed on average 7–9 years later. Of the 3,250 patients, 1,880 (57.8%) returned for examination [1, 2, 7]. At follow-up, a cross-sectional nested case-control study of markers and precipitators of inflammation and endothelial function and their associations with complications was performed (n=543). Markers of inflammation could not be determined at baseline because these samples have run out.
We assessed microvascular complications and cardiovascular disease; did a physical examination; measured height, weight, waist and hip circumference, and resting blood pressure; obtained information on smoking habits; and measured biochemical variables according to a standardised protocol [6]. Albumin excretion rates were measured centrally from 2×24-h urine collections as previously described [1]. Micro- and macroalbuminuria were defined as an albumin excretion rate of between 20 and 200, and above 200 μg/min, respectively. We estimated glomerular filtration rate (GFR) by the Cockroft–Gault formula. Retinopathy was assessed from retinal photographs according to the EURODIAB protocol [8]. Cardiovascular disease was defined as a positive medical history of a cardiovascular event, including myocardial infarction, angina, coronary artery bypass graft and/or stroke, and/or ischaemic changes on a centrally Minnesota coded ECG [9]. Hypertension was defined as systolic pressure ≥140 mmHg, diastolic pressure ≥90 mmHg and/or use of antihypertensive drugs.
Laboratory measurements
Pentosidine levels were determined in unhydrolysed urine as previously described [10]. Urinary excretion of pentosidine was normalised for urine concentration by expressing it as nmol pentosidine/mmol urinary creatinine. CML and CEL were determined in plasma as previously described [11] with an inter-assay coefficient of variation of 6.0%. CML and CEL were normalised for lysine concentration by expressing it as μM/mM lysine.
Plasma levels of CRP (n=539), IL-6 (n=536) and TNF-α (n=528) were measured as previously described [12]. Intra- and inter-assay coefficients of variation as determined in our laboratory were 3.9 and 8.7%, 4.5 and 9.0%, 7.3 and 8.5%, respectively.
Selection of cases and controls
Cases were selected to have the greatest complication burden as possible, to provide sufficient numbers for subgroup analyses. Controls were selected to be completely free of complications. Thus cases were all those with cardiovascular disease or proliferative retinopathy or macroalbuminuria at follow-up, and all those with microalbuminuria and some degree of retinopathy (n=348). Controls were all those who had no evidence of cardiovascular disease, retinopathy or neuropathy, and were normoalbuminuric at follow-up (n=195). This selection allowed us to compare people with and without complications. Cases and controls were unmatched, so that the impact of key variables, such as age, could still be assessed, and any adjustments were taken care of at the analysis stage.
Z-score
Because we measured markers of inflammatory activity only once, the associations (if any) of inflammatory activity with outcomes will tend to be underestimated. To address this concern, we constructed an inflammatory marker Z-score that combined information on C-reactive protein, interleukin-6 and tumour necrosis factor-α. For each individual, the values of each inflammation marker were expressed as a Z-score, i.e. (value in the individual minus the mean value in the study population) divided by the standard deviation, a value that thus ranged from approximately −2.5 to +2.5. The inflammatory marker Z-score was then calculated as (Z-score of C-reactive protein+Z-score of interleukin-6+Z-score of tumour necrosis factor-α) / 3.
Statistical analysis
For the subsequent analyses, we divided the patients into groups according to the level of albuminuria (normo-, micro- and macroalbuminuria), the presence and severity of retinopathy (no, non-proliferative and proliferative), and the presence or absence of cardiovascular disease. In the latter group, we excluded from the analyses those in whom cardiovascular disease was absent but who did have micro- or macroalbuminuria or retinopathy (227 of 348 individuals).
Primary analyses
Variables with a skewed distribution were ln-transformed in all analyses. We used ANOVA to estimate mean values of CRP, IL-6, TNF-α and the inflammatory marker Z-score according to the presence or absence and severity of vascular complications. We then adjusted these analyses for age, sex, HbA1c, duration of diabetes and systolic blood pressure. We used linear regression analyses to investigate the association of inflammatory markers with GFR.
Secondary analyses
We next investigated whether HbA1c, pentosidine, CML, CEL, systolic blood pressure and other vascular risk factors were associated with albuminuria, GFR, retinopathy and cardiovascular disease independently of age, sex, HbA1c, duration of diabetes and systolic blood pressure, and whether these associations were mediated by the level of inflammatory activity, by further adjusting these associations for the inflammatory marker Z-score. A change in the β of more than 33% was considered to be consistent with mediation by the inflammatory marker Z-score.
To compare the strength of the association of the inflammatory marker Z-score with vascular complications with that of established risk factors, we performed logistic regression analyses with the presence of vascular complications as dependent and the inflammatory marker Z-score and HbA1c as independent variables.
A p-value of <0.05 was considered statistically significant.
Results
Table 1 shows the baseline characteristics of the study population.
Primary analyses
All inflammatory markers were significantly associated with albuminuria, GFR (inversely), retinopathy and cardiovascular disease in crude and adjusted analyses, except for CRP and albuminuria, CRP and GFR, and IL-6 and GFR in the adjusted analyses (Tables 2, 3, 4, 5 and Fig. 1).
Secondary analyses
HbA1c, systolic blood pressure, total cholesterol, triglycerides, LDL cholesterol, duration of diabetes and pack-years of smoking were independently associated with albuminuria and with retinopathy. Body mass index and HDL cholesterol were independently associated with retinopathy. Pentosidine was associated only with albuminuria; the association with retinopathy disappeared after adjustment for duration of diabetes. CML was independently associated only with albuminuria, while CEL was not associated with albuminuria, retinopathy or cardiovascular disease. Pentosidine, CML, CEL, body mass index, waist circumference, hypertension and duration of diabetes were independently associated with GFR (Table 5). None of the above associations changed markedly by adjustment for the inflammatory marker Z-score, except for the association of triglycerides with macroalbuminuria, and the associations of triglycerides, body mass index and HDL cholesterol with retinopathy (Table 6).
HbA1c, HDL cholesterol, triglycerides, duration diabetes and pack-years of smoking were independently associated with cardiovascular disease, but these associations were not notably affected by adjustment for the inflammatory marker Z-score.
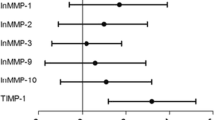
The association of the inflammatory marker Z-score with vascular complications was of a similar order of magnitude as that of HbA1c (Fig. 2).
The odds ratios of the associations of HbA1c and the inflammatory marker Z-score with albuminuria, retinopathy and cardiovascular disease. The association of the inflammatory marker Z-score with the presence of vascular complications was somewhat smaller than, but of a similar magnitude as, the association of HbA1c with the presence of vascular complications. Odds ratios were calculated per standard deviation (SD)
Additional adjustments
The results were not changed materially by additional adjustments for body mass index, waist circumference, total cholesterol, triglycerides, HDL and LDL cholesterol, serum creatinine, pack-years of smoking, the presence of albuminuria, retinopathy or cardiovascular disease, the use of analgesics and anti-inflammatory drugs (n=59), oral contraceptives (n=110) or hormone replacement therapy (n=38), and the presence of peripheral artery disease as assessed by the ankle arm index, or exclusion of individuals with CRP levels above 10 mg/l (n=16), except that the association between CRP and retinopathy decreased after adjustment for body mass index (Table 3, model 2).
Discussion
Our study shows that inflammatory activity is associated with vascular complications in Type 1 diabetic individuals. Due to the cross-sectional design, we cannot establish whether these associations are causal. However, our data are consistent with the hypothesis that inflammation is involved in the pathogenesis of both small and large vessel disease. Our results further suggest that inflammatory activity is involved in the pathway through which dyslipidaemia and obesity lead to microvascular damage.
Inflammation may contribute to increased urinary albumin excretion and decreased GFR by increasing glomerular permeability [13–15]. In support, anti-inflammatory therapy can prevent the development of albuminuria in experimental diabetic nephropathy [16]. In advanced nephropathy, which is often associated with a decline in GFR, renal tubular protein overload has been shown to elicit an inflammatory response that eventually results in renal interstitial remodelling and scarring [17]. In this phase, the kidney in diabetes may thus be both a target and a source of inflammation, a notion that is consistent with our observation of a stronger association of inflammation with macro- than with microalbuminuria.
Dyslipidaemia can damage glomerular podocytes, and mesangial and endothelial cells through exposure to oxidised LDL [18]. Activation of these cells results in an inflammatory response [19]. Our data suggest that the association of elevated triglyceride levels with albuminuria is, in part, mediated by inflammation.
AGEs are thought to contribute to the pathogenesis of diabetic complications in part through inflammatory mechanisms [20]. We measured pentosidine, a specific marker of glycation [21, 22], urinary levels of which have been shown to be closely related to serum concentrations [23], and CML and CEL, which are thought to be major AGE products but which can be formed independently of glycation [24]. However, the associations of pentosidine and CML with albuminuria appeared not to be mediated through inflammation. Other pathogenic pathways, such as those involving matrix function and oxidative stress, may thus be involved [24]. The inverse associations of pentosidine, CML and CEL with GFR suggest that these AGEs are important in the pathogenesis of the decline in GFR in diabetic nephropathy, and evidence exists that inhibitors of AGE formation have renoprotective effects [25]. Alternatively, we cannot exclude the possibility that levels of AGEs were increased due to the decrease in GFR.
Inflammatory markers were associated with both early and advanced retinopathy, which suggests that inflammation plays a role in both early and late stages of diabetic retinopathy. The interpretation that the retina is a source of inflammation is unlikely, as the retina is unable to increase protein synthesis to the extent that plasma protein levels increase [26]. Our results are in accordance with previous studies that suggest a role for inflammation and endothelial dysfunction in the pathophysiology of diabetic retinopathy [27, 28]. Inflammatory mediators may increase retinal vascular permeability [29], possibly by upregulation of adhesion molecules on endothelial cells, and may cause changes in endothelial cell contact with pericytes, resulting in pericyte loss and the development of microaneurysms [30]. In the pathogenesis of proliferative retinopathy, retinal ischaemia and subsequent neovascularisation play a pivotal role. Increased inflammatory activity has been shown to stimulate leucocytes to adhere to retinal endothelial cells [30], which causes leucostasis and temporary ischaemia upstream of the adhering leucocytes. Reperfusion may damage the endothelium due to the generation of oxidative stress [31], setting the stage for a vicious cycle of endothelial dysfunction, ischaemia and reperfusion. Alternatively, inflammation may reduce endothelial production of nitric oxide [14]. Together with an increased release of vasoconstrictors, this may lead to vasospasm and subsequent retinal ischaemia [32]. In addition, treatment with anti-inflammatory agents may decrease the elevated retinal TNF-α levels in diabetes [33].
The association of body mass index with retinopathy appeared, in part, mediated by inflammation. Fat cells are a potential source of inflammatory mediators [34]. Importantly, our data suggest that even at low body mass indexes, as in our population, body fat and its distribution play a role in the development of microvascular complications.
Low HDL cholesterol levels are associated with retinopathy [2]. Our data suggest that this association is, in part, mediated by inflammation. Dyslipidaemia may lead to a systemic increase of the inflammatory state by glomerulosclerotic and atherosclerotic processes as described above [19]. However, we clearly cannot exclude the reverse interpretation that increased inflammatory activity causes changes in lipid profile [35], as prospective studies are needed to do this.
We observed an association between inflammation and the presence of cardiovascular disease in type 1 diabetic individuals. Inflammatory markers may reflect low-grade vessel wall inflammation, which plays a pivotal role in the pathogenesis of cardiovascular disease [19]. The reverse interpretation, that cardiovascular disease leads to an increased inflammatory activity is unlikely, since there is much evidence that inflammation is involved in the pathophysiology of cardiovascular disease [19]. Alternatively, body fat [34] or, in the presence of advanced nephropathy, the kidney may be sources of inflammatory mediators in diabetes. In any case, low-grade inflammation increases the expression of vascular adhesion molecules on endothelial cells, enhances the invasion of monocytes into the vascular wall, and eventually leads to the formation of atherosclerosis and cardiovascular disease [19].
Due to the cross-sectional design of this study, we cannot establish the time course of the associations between inflammation and vascular complications. However, longitudinal studies in non-diabetic and type 2 diabetic individuals have demonstrated that the increase in inflammatory activity is progressive and precedes the occurrence of vascular complications [36]. At this time, no longitudinal data of this type exist in type 1 diabetes. Therefore this cross-sectional study may serve as a starting point to explore these associations in type 1 diabetes. The probability of confounding in the associations we explored has been minimised by adjustments for many possible confounders. However, interference by factors we did not measure, such as other AGEs, cannot be ruled out. In addition, concentrations of inflammatory markers were only measured once, which might have diluted the associations we found, which thus may to some extent have been underestimated. The validity of our study design is supported by the finding that conventional risk factors were, as expected [37, 38], associated with microvascular complications and cardiovascular disease.
In conclusion, inflammation is associated with microvascular complications and cardiovascular disease in type 1 diabetes. These associations were of a similar order of magnitude as the association HbA1c with vascular complications (Fig. 2). In addition, the associations of obesity and dyslipidaemia with vascular complications appear dependent on inflammatory activity. This suggests that inflammation itself is involved in the pathophysiological pathway leading to vascular complications and that it is involved in the pathways through which obesity and dyslipidaemia lead to vascular complications. Therefore, strategies to decrease inflammatory activity may help to prevent the development of vascular complications in type 1 diabetes.
Abbreviations
- CEL:
-
\({\text{N}}^{\varepsilon } \)-(carboxyethyl)lysine
- CML:
-
\({\text{N}}^{\varepsilon } \)-(carboxymethyl)lysine
- CRP:
-
C-reactive protein
References
Chaturvedi N, Bandinelli S, Mangili R et al (2001) Microalbuminuria in type 1 diabetes: rates, risk factors and glycemic threshold. Kidney Int 60:219–227
Chaturvedi N, Sjoelie AK, Porta M et al (2001) Markers of insulin resistance are strong risk factors for retinopathy incidence in type 1 diabetes. Diabetes Care 24:284–289
Ridker PM, Hennekens CH, Buring JE, Rifai N (2000) C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 342:836–843
Schalkwijk CG, Poland DC, van Dijk W et al (1999) Plasma concentration of C-reactive protein is increased in type I diabetic patients without clinical macroangiopathy and correlates with markers of endothelial dysfunction: evidence for chronic inflammation. Diabetologia 42:351–357
Schmidt AM, Hori O, Chen JX et al (1995) Advanced glycation endproducts interacting with their endothelial receptor induce expression of vascular cell adhesion molecule-1 (VCAM-1) in cultured human endothelial cells and in mice. A potential mechanism for the accelerated vasculopathy of diabetes. J Clin Invest 96:1395–1403
The EURODIAB IDDM Complications Study Group (1994) Microvascular and acute complications in IDDM patients: the EURODIAB IDDM complications study. Diabetologia 37:278–285
Chaturvedi N, Fuller JH, Taskinen MR, The EURODIAB Prospective Complications Study Group (2001) Differing associations of lipid and lipoprotein disturbances with the macrovascular and microvascular complications of type 1 diabetes. Diabetes Care 24:2071–2077
Aldington SJ, Kohner EM, Meuer S, Klein R, Sjolie AK, The EURODIAB IDDM Complications Study Group (1995) Methodology for retinal photography and assessment of diabetic retinopathy: the EURODIAB IDDM complications study. Diabetologia 38:437–444
Koivisto VA, Stevens LK, Mattock M et al (1996) Cardiovascular disease and its risk factors in IDDM in Europe. EURODIAB IDDM Complications Study Group. Diabetes Care 19:689–697
Smulders RA, Stehouwer CD, Schalkwijk CG, Donker AJ, Van Hinsbergh VW, TeKoppele JM (1998) Distinct associations of HbA1c and the urinary excretion of pentosidine, an advanced glycosylation end-product, with markers of endothelial function in insulin-dependent diabetes mellitus. Thromb Haemost 80:52–57
Lieuw-a-Fa M, Van Hinsbergh VW, Teerlink T et al (2004) Increased levels of \({\text{N}}^{\varepsilon } \)-(carboxymethyl)lysine and \({\text{N}}^{\varepsilon } \)-(carboxyethyl)lysine in type 1 diabetic patients with impaired renal function: correlation with markers of endothelial dysfunction. Nephrol Dial Transplant 19:631–636
Schram MT, Chaturvedi N, Schalkwijk C et al (2003) Vascular risk factors and markers of endothelial function as determinants of inflammatory markers in type 1 diabetes: the EURODIAB Prospective Complications Study. Diabetes Care 26:2165–2173
Ling BN, Matsunaga H, Ma H, Eaton DC (1995) Role of growth factors in mesangial cell ion channel regulation. Kidney Int 48:1158–1166
Kim F, Gallis B, Corson MA (2001) TNF-alpha inhibits flow and insulin signaling leading to NO production in aortic endothelial cells. Am J Physiol, Cell Physiol 280:C1057–C1065
Oragui EE, Nadel S, Kyd P, Levin M (2000) Increased excretion of urinary glycosaminoglycans in meningococcal septicemia and their relationship to proteinuria. Crit Care Med 28:3002–3008
Utimura R, Fujihara CK, Mattar AL, Malheiros DM, De LNI, Zatz R (2003) Mycophenolate mofetil prevents the development of glomerular injury in experimental diabetes. Kidney Int 63:209–216
Remuzzi G, Bertani T (1998) Pathophysiology of progressive nephropathies. N Engl J Med 339:1448–1456
Joles JA, Kunter U, Janssen U et al (2000) Early mechanisms of renal injury in hypercholesterolemic or hypertriglyceridemic rats. J Am Soc Nephrol 11:669–683
Ross R (1999) Atherosclerosis—an inflammatory disease. N Engl J Med 340:115–126
Schmidt AM, Stern DM (2001) Receptor for age (RAGE) is a gene within the major histocompatibility class III region: implications for host response mechanisms in homeostasis and chronic disease. Front Biosci 6:D1151–D1160
Sugiyama S, Miyata T, Ueda Y et al (1998) Plasma levels of pentosidine in diabetic patients: an advanced glycation end product. J Am Soc Nephrol 9:1681–1688
Beisswenger PJ, Moore LL, Curphey TJ (1993) Relationship between glycemic control and collagen-linked advanced glycosylation end products in type I diabetes. Diabetes Care 16:689–694
Yoshihara K, Nakamura K, Kanai M et al (1998) Determination of urinary and serum pentosidine and its application to elder patients. Biol Pharm Bull 21:1005–1008
Bierhaus A, Hofmann MA, Ziegler R, Nawroth PP (1998) AGEs and their interaction with AGE-receptors in vascular disease and diabetes mellitus. I. The AGE concept. Cardiovasc Res 37:586–600
Forbes JM, Soulis T, Thallas V et al (2001) Renoprotective effects of a novel inhibitor of advanced glycation. Diabetologia 44:108–114
Franken AA, Derkx FH, Man in’t Veld AJ et al (1990) High plasma prorenin in diabetes mellitus and its correlation with some complications. J Clin Endocrinol Metab 71:1008–1015
Elner SG, Elner VM, Jaffe GJ, Stuart A, Kunkel SL, Strieter RM (1995) Cytokines in proliferative diabetic retinopathy and proliferative vitreoretinopathy. Curr Eye Res 14:1045–1053
Limb GA, Hollifield RD, Webster L, Charteris DG, Chignell AH (2001) Soluble TNF receptors in vitreoretinal proliferative disease. Invest Ophthalmol Vis Sci 42:1586–1591
Claudio L, Martiney JA, Brosnan CF (1994) Ultrastructural studies of the blood-retina barrier after exposure to interleukin-1 beta or tumor necrosis factor-alpha. Lab Invest 70:850–861
Porta M (1996) Endothelium: the main actor in the remodelling of the retinal microvasculature in diabetes. Diabetologia 39:739–744
Kohner EM, Patel V, Rassam SM (1995) Role of blood flow and impaired autoregulation in the pathogenesis of diabetic retinopathy. Diabetes 44:603–607
Chakravarthy U, Gardiner TA (1999) Endothelium-derived agents in pericyte function/dysfunction. Prog Retin Eye Res 18:511–527
Joussen AM, Poulaki V, Mitsiades N et al (2002) Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-alpha suppression. FASEB J 16:438–440
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 148:209–214
Kreisberg RA (1998) Diabetic dyslipidemia. Am J Cardiol 82:67U–73U
Stehouwer CD, Gall MA, Twisk JW, Knudsen E, Emeis JJ, Parving HH (2002) Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes 51:1157–1165
Ebeling P, Koivisto VA (1997) Occurrence and interrelationships of complications in insulin-dependent diabetes in Finland. Acta Diabetol 34:33–38
Baynes JW, Thorpe SR (1999) Role of oxidative stress in diabetic complications: a new perspective on an old paradigm. Diabetes 48:1–9
Acknowledgements
We would like to thank all the investigators and patients who very kindly participated in the study. The EURODIAB PCS was supported by grants from the Wellcome Trust, the European Community and Diabetes UK. C.G. Schalkwijk was supported by a grant from the Diabetes Fonds Nederland. There were no conflicts of interest.
The EURODIAB Prospective Complications Study Group
B. Karamanos, A. Kofinis, K. Petrou, Hippokration Hospital, Athens, Greece. F. Giorgino, L. Laviola, G. De Pergola, G. Picca, A. Angarano, R. Giorgino, Medicina Interna, Endocrinologia e Malattie Metaboliche D.E.T.O. Università degli Studi di Bari, Bari, Italy. C. Ionescu-Tirgoviste, A. Cosma, C. Guja, Clinic of Diabetes, Nutrition & Metabolic Diseases, Bucharest, Romania. M. Songini, A. Casu, M. Pedron, S. Pintus, M. Fossarello*, Diabetes Unit, Ospedale San Michele, Ophthalmology Department*, Cagliari, Italy. J.B. Ferriss, G. Grealy, D.O. Keefe, Cork Regional Hospital, Cork, Ireland. M. Toeller, C. Arden, Diabetes Research Institute, Heinrich-Heine University, Düsseldorf, Germany. R. Rottiers, C. Tuyttens, H. Priem, University Hospital of Gent, Belgium. P. Ebeling, M. Kylliäinen, V.A. Koivisto, University Hospital of Helsinki, Finland. B. Idzior-Walus, J. Sieradzki, K. Cyganek, B. Solnica, Department of Metabolic Diseases, Jagiellonian University, Krakow, Poland. H.H.P.J. Lemkes, M. Krans, University Hospital of Leiden, The Netherlands. J. Nunes-Correa, M.C. Rogado, L. Gardete-Correia, M.C. Cardoso, A. Silva, J. Boavida, M. Machado Sa Marques, Portuguese Diabetic Association, Lisbon, Portugal. G. Michel, R. Wirion, S. Cardillo, Centre Hospitalier, Luxembourg. G. Pozza, R. Mangili, V. Asnaghi, Ospedale San Raffaele, Milan, Italy. E. Standl, B. Schaffler, H. Brand, A. Harms, City Hospital Schwabing, Munich, Germany. D. Ben Soussan, O. Verier-Mine, P. Fallas, M.C. Fallas, Centre Hospitalier de Valenciennes, France. J.H. Fuller, J. Holloway, L. Asbury, D.J. Betteridge, University College London, UK. G. Cathelineau, A. Bouallouche, B. Villatte Cathelineau, Hospital Saint-Louis, Paris, France. F. Santeusanio, G. Rosi, V. D’Alessandro, C. Cagini, P. Bottini, P. Reboldi, Instituto di Patologia Medica, Policlinico, Perugia, Italy. R. Navalesi, G. Penno, S. Bandinelli, R. Miccoli, M. Nannipieri, Dipartimento di Endocrinologia e Metabolismo, Pisa, Italy. G. Ghirlanda, C. Saponara, P. Cotroneo, A. Manto, A. Minnella, Universita Cattolica del Sacro Cuore, Rome, Italy. J.D. Ward, S. Tesfaye, S. Eaton, C. Mody, Royal Hallamshire Hospital, Sheffield, UK. M. Borra, P. Cavallo Perin, S. Giunti, G. Grassi, G.F. Pagano, M. Porta, R. Sivieri, F. Vitelli, D. Ferrari, Dipartimento di Medicina Interna, Università di Torino and ASO CTO/CRF/Maria Adelaide, Turin, Italy. N. Papazoglou, G. Manes, General Hospital of Thessaloniki, Greece. M. Muggeo, M. Iagulli, V. Cattedra, Vittorio Cacciatori, di Malattie del Metabolismo, Verona, Italy. K. Irsigler, H. Abrahamian, Hospital Vienna Lainz, Austria. S. Walford, J. Sinclair, S. Hughes, J. Ward, New Cross Hospital, Wolverhampton, UK. G. Roglic, Z. Metelko, Z.R. Pepeonik, Vuk Vrhovac Institute for Diabetes, Zagreb, Croatia.
Steering Committee Members: J.H. Fuller (London), B. Karamanos, Chairman (Athens), A.K. Sjolie (Aarhus), N. Chaturvedi (London), M. Toeller (Dusseldorf), G. Pozza Co-chairman (Milan), B. Ferriss (Cork), M. Porta (Turin), R. Rottiers (Gent), G. Michel (Luxembourg).
Co-ordinating Centre: J.H. Fuller, N. Chaturvedi, J. Holloway, D. Webb, University College London.
Central Laboratories: G.C. Viberti, R. Swaminathan, P. Lumb, A. Collins, S. Sankaralingham, Guy’s and St Thomas’ Hospital, London, UK.
Retinopathy Grading Centre: S. Aldington, T. Mortemore, H. Lipinski, Royal Postgraduate Medical School of Imperial College London, London, UK
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Schram, M.T., Chaturvedi, N., Schalkwijk, C.G. et al. Markers of inflammation are cross-sectionally associated with microvascular complications and cardiovascular disease in type 1 diabetes—the EURODIAB Prospective Complications Study. Diabetologia 48, 370–378 (2005). https://doi.org/10.1007/s00125-004-1628-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1628-8