Abstract
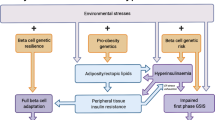
The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes have been debated extensively. The concept that a feedback loop governs the interaction of the insulin-sensitive tissues and the beta cell as well as the elucidation of the hyperbolic relationship between insulin sensitivity and insulin secretion explains why insulin-resistant subjects exhibit markedly increased insulin responses while those who are insulin-sensitive have low responses. Consideration of this hyperbolic relationship has helped identify the critical role of beta-cell dysfunction in the development of Type 2 diabetes and the demonstration of reduced beta-cell function in high risk subjects. Furthermore, assessments in a number of ethnic groups emphasise that beta-cell function is a major determinant of oral glucose tolerance in subjects with normal and reduced glucose tolerance and that in all populations the progression from normal to impaired glucose tolerance and subsequently to Type 2 diabetes is associated with declining insulin sensitivity and beta-cell function. The genetic and molecular basis for these reductions in insulin sensitivity and beta-cell function are not fully understood but it does seem that body-fat distribution and especially intra-abdominal fat are major determinants of insulin resistance while reductions in beta-cell mass contribute to beta-cell dysfunction. Based on our greater understanding of the relative roles of insulin resistance and beta-cell dysfunction in Type 2 diabetes, we can anticipate advances in the identification of genes contributing to the development of the disease as well as approaches to the treatment and prevention of Type 2 diabetes.
Similar content being viewed by others
Introduction
The pathogenesis of Type 2 diabetes has been studied extensively. In the course of this work it has become abundantly clear that by the time hyperglycaemia develops, reductions in both insulin sensitivity and beta-cell function have already occurred [1]. While it is clear that hyperglycaemia is associated with both insulin resistance and beta-cell dysfunction, there has been much debate over the past few decades regarding the relative importance of these two abnormalities. Many groups have suggested that insulin resistance is the primary abnormality and that beta-cell dysfunction is a late event that arises from the prolonged, increased secretory demand placed on the beta cell by insulin resistance [2, 3]. In contrast, others have suggested that reduced beta-cell function, manifest as decreased insulin release, is a prerequisite for the progression from NGT to hyperglycaemia [4, 5, 6].
This disagreement over the relative importance of insulin resistance versus beta-cell dysfunction is partly due to the fact that evaluation of these parameters has frequently been done in isolation. This approach does not take into account the fact that glucose homeostasis, as is the case for most endocrine systems, is vitally dependent on a feedback system. Once consideration is given to the presence of a tightly regulated feedback system incorporating the beta cell and the insulin-sensitive tissues, it becomes abundantly clear that reductions in both insulin sensitivity and beta-cell function are present early in the course of the development of Type 2 diabetes.
This review will focus on the importance of insulin resistance and beta-cell dysfunction in the pathogenesis of Type 2 diabetes. In the course of the discussion, it will be apparent that changes in beta-cell function are both an early and critical component in the pathogenesis of the hyperglycaemia of Type 2 diabetes.
The natural history of Type 2 diabetes
It is now well established that the development of Type 2 diabetes results from an interaction of a subject's genetic makeup and their environment, and that with the increasing prevalence of obesity [7], the prevalence of diabetes is reaching epidemic proportions [8]. The development of obesity seems to be an important factor portending the development of insulin resistance [9, 10], which in the presence of a genetically determined propensity to beta-cell dysfunction results in alterations in glucose tolerance. Unfortunately, while it had previously been considered that Type 2 diabetes was essentially a disease of middle aged and older subjects and that it took years to develop, this concept is currently undergoing re-evaluation. This is due to the emergence of Type 2 diabetes as a new and very serious health problem in children [11, 12]. It is of interest that the limited studies currently carried out in these children suggest the co-existence of obesity, insulin resistance and beta-cell dysfunction as occurs in older Type 2 diabetic patients [13].
Historically, clinicians have found that controlling hyperglycaemia in Type 2 diabetes can be difficult, frequently requiring increasing doses of oral antidiabetic agents and the addition of insulin. This progressive nature of Type 2 diabetes has been further highlighted by two recent, large clinical studies performed on opposite sides of the Atlantic. In the United Kingdom Prospective Diabetes Study (UKPDS), despite treatments to establish euglycaemia in the intensive policy group, glycaemic control deteriorated so that additional pharmacological therapy was required. Thus, after 9 years only 25% of the subjects in the intensive treatment arm were achieving a HbA1c of less than 7% with monotherapy alone [14, 15]. Recently, the Diabetes Prevention Program (DPP) reported that in subjects with IGT, an intensive lifestyle intervention and metformin reduced the rate of development of diabetes by 58% and 31%, respectively compared to placebo [16]. This large study which involved more than 1 000 subjects in each arm also showed that in subjects with IGT, the natural history was a continued progressive deterioration of glycaemia so that the fasting plasma glucose concentration and HbA1c increased over time. The basis for progression in the UKPDS was examined using the Homeostasis Model Assessment (HOMA) which suggested that in this cohort of subjects with recently diagnosed Type 2 diabetes, an ongoing decline in beta-cell function without a change in insulin sensitivity was occurring [17, 18]. The underlying cause of the progression from IGT to diabetes in subjects in the DPP has not yet been reported. Based on data that will be discussed subsequently, one can anticipate that a loss of beta-cell function will also be observed at this earlier stage in the natural history of the disease and that insulin resistance may make an additional contribution. In addition, our current understanding of the contribution of obesity and body fat distribution to insulin sensitivity will be further elucidated by examination of the data collected in the DPP.
Determinants of insulin sensitivity and the importance of body fat distribution
Despite tremendous advances in molecular biology and the continued identification of increasingly more molecules involved in the insulin signalling cascade [19], the molecular mechanism(s) that underlies the development of insulin resistance in humans still remains elusive. What has become apparent is that insulin sensitivity is influenced by a number of different factors such as genetics [20], age [21, 22], acute exercise [23], physical fitness [24], dietary nutrients [25], medications [26, 27, 28], obesity [9, 10, 29, 30, 31, 32] and body fat distribution [31, 33, 34, 35, 36, 37, 38]. A discussion of some of these follows.
Examination of groups of healthy subjects in a number of different populations has shown that known genetic mutations associated with insulin resistance are rare [20, 39, 40, 41, 42, 43, 44]. For instance, in a cohort of markedly insulin-resistant subjects, two different dominant negative mutations of the peroxisome proliferator activating receptor gamma (PPAR-γ) receptor could only explain less than 4% of these cases [20], with the effect of this mutation on obesity and diabetes being debated [45, 46, 47]. From this it seems unlikely that a single genetic alteration explains a large number of the "garden variety" cases of insulin resistance. Rather, it is more likely that a number of different genes may contribute, some of which may be obesity genes.
Three commonly encountered examples of factors that influence insulin sensitivity but are apparently not genetically determined are aging, exercise and dietary constituents. Aging is typically associated with diminished insulin sensitivity [21, 22]. Exercise is more complex because it has both acute and chronic effects, both of which are capable of improving insulin sensitivity [23, 24]. However, even the long term effect of exercise training on insulin sensitivity is relatively short lived, waning significantly within a few days after stopping regular exercise [23, 48]. Dietary constituents have also been shown to modulate insulin sensitivity. This effect is partly related to age, with aging being associated with a decline in the body's responsiveness to carbohydrate [25, 49]. Thus, the typical Western diet tends to promote a reduction in insulin sensitivity that is not fully explained by the obesity that is commonly associated with the consumption of these diets that contain increased fat. Conversely, the consumption of increased amounts of carbohydrate is associated with an increase in insulin sensitivity within a period as short as 3 days [49], and in improved glucose tolerance particularly in the elderly [25, 49] and those with Type 2 diabetes [50]. Finally, a number of medications including corticosteroids [26], growth hormone [27] and nicotinic acid [28] have all been shown to induce insulin resistance. However, even when the effects of age, diet and exercise are considered as potential explanations for differences in insulin sensitivity, there is still a large residual variation that has to be related to other factors. We believe that a major component of this residual variation is related to obesity, but more importantly to differences in body fat distribution.
It is well recognised that obesity is an important determinant of insulin sensitivity [9, 10, 29, 30, 31, 32]. Body-fat distribution, however, seems to be a critical aspect. Central body fat accumulation is associated with insulin resistance whereas peripheral body fat accumulation seems to be of less critical importance. Whereas it is generally agreed that central deposition of fat is of greater importance metabolically [31, 51, 52], there has been some debate about the relative roles of the different central depots in determining insulin sensitivity. Several groups have made a strong case that the intra-abdominal depot is the primary correlate of insulin sensitivity [31, 33, 35], while others have proposed that the central subcutaneous fat depot is the major factor determining a reduction in insulin sensitivity [36, 53].
To examine central fat distribution, investigators have used computed tomography (CT) or magnetic resonance imaging (MRI). Using CT scans, we found that visceral or intra-abdominal fat is better correlated with insulin resistance than centrally located subcutaneous fat. In our initial study of a small cohort of Japanese American men, we did not find a relationship between insulin sensitivity and BMI but did find that the quantity of intra-abdominal fat was related to insulin sensitivity [35]. Based on our work with 93 young, apparently healthy subjects [54] and on our more recent studies in a group of 174 subjects (73 men / 101 women) with a broad age range (30–75 years) [38], it has become apparent that the relationship between BMI and insulin sensitivity is non-linear, rather than linear as had been traditionally thought. As with BMI, the relationship between insulin sensitivity and subcutaneous fat or intra-abdominal fat was non-linear, with intra-abdominal fat being most strongly correlated explaining 47% of the variance in insulin sensitivity. The importance of intra-abdominal fat in the determination of insulin sensitivity was further highlighted by the fact that it was the most important contributor to insulin sensitivity in a multiple regression model that included subcutaneous fat, WHR and BMI.
Further analyses of the data from these 174 subjects has provided information on other aspects related to central body fat distribution, insulin sensitivity and the two adipose tissue derived peptides, leptin and adiponectin [38, 55]. First, sex does not seem to affect the relationship between the quantity of intra-abdominal fat and insulin sensitivity (Fig. 1A). Second, the individual data demonstrated a large degree of overlap in the amount of intra-abdominal fat between insulin-resistant subjects with lower and higher BMI, based on a cutpoint of 25 kg/m2 (Fig. 1B). Thus, some of the leaner subjects were insulin-resistant and had large amounts of intra-abdominal fat while some of the more obese subjects were insulin-resistant and had relatively small amounts of intra-abdominal fat. These findings are in keeping with the fact that a number of factors besides intra-abdominal fat determine insulin sensitivity. Third, whereas intra-abdominal fat is a major determinant of insulin sensitivity, subcutaneous fat seems to be the major contributor to plasma leptin concentrations. This finding suggests that the concurrent accumulation of fat in these two depots is responsible for the insulin resistance and increased plasma leptin concentrations typically observed in most obese subjects. It also does not seem that insulin sensitivity per se is a major determinant of plasma leptin concentrations. Fourth, adiponectin, an adipose tissue-derived protein in which there has recently been great interest because of its potential role in the determination of insulin sensitivity [56, 57], is more strongly inversely related to intra-abdominal than to subcutaneous fat [55, 56]. Further, as with leptin, plasma adiponectin concentrations are higher in women than in men [55, 58]. However, it is unclear whether this sex-based difference in adiponectin concentrations is related to the fact that women have greater amounts of body fat than men [59]. Future studies will determine the potential role of adiponectin in the pathogenesis of insulin resistance as it relates to obesity and its associated disorders.
The relationship between the insulin sensitivity index (SI) and intra-abdominal fat (IAF) area in 174 subjects subdivided based on (A) sex (73 men, solid circle; 101 women, open square) and (B) a BMI of 25 kg/m2, (78 with a BMI<25 kg/m2, solid diamond; 96 with a BMI≥25 kg/m2, triangle). The relationship between these two variables is non-linear (r2=0.473, p<0.001), with the relationship in men and women being similar. In subjects classified based on body size, even those who would be considered as normal (BMI<25 kg/m2) can have large amounts of IAF and some who are overweight or obese can have small amounts of IAF. Adapted from [38]
If the intra-abdominal fat depot were an important determinant of insulin sensitivity, one would predict that interventions that reduce the mass of adipose tissue within the peritoneal cavity should be associated with improvements in insulin sensitivity. This was shown to be the case in studies involving weight loss or exercise training. As mentioned, older subjects are insulin resistant and have increased central adiposity, especially visceral fat [60]. In a study of 21 older men, a 3-month weight loss program was associated with an average 10 kg (10%) weight loss, of which 80% was fat. This reduction in fat mass was associated with a 24% reduction in intra-abdominal fat area, a 58% improvement in insulin sensitivity and the development of a less atherogenic lipid profile [61]. Similar findings were reported by Goodpaster et al [37] who also examined total fat and fat-free mass and found that these parameters decreased along with a reduction in thigh muscle fat. The outcomes of a study involving older men who underwent a 6-month exercise training program also support the importance of intra-abdominal fat as a determinant of insulin sensitivity. In this study exercise training resulted in a 25% reduction in intra-abdominal fat area and a 36% improvement in insulin sensitivity [24, 62]. The findings are, however, hard to interpret as fat was also lost from peripheral sites such as the thigh and because exercise per se can improve insulin sensitivity [23]. Of additional interest and in support of the role of intra-abdominal fat as a determinant of insulin sensitivity is the observation that the thiazolidinediones, which induce adipocyte differentiation [63], not only improve insulin sensitivity but also increase fat deposition in the subcutaneous rather than the intra-abdominal fat compartment [64, 65]. These PPAR-γ agonists have also been shown to "favorably" alter the plasma concentrations of adipocyte-derived proteins by decreasing resistin [66] and increasing adiponectin [67].
Against this background it seems that an important factor in determining insulin sensitivity in apparently healthy men and women is central adiposity, and specifically intra-abdominal fat accumulation. While it is unclear what is the mechanism(s) by which body-fat distribution influences insulin sensitivity, the continued recognition of adipose tissue as an active endocrine organ suggests that a fat produced molecule may well be an important mediator of changes in insulin sensitivity. What is clear is that differences in the deposition of fat and secretion of molecules from these depots explains much of the variability in these parameters in healthy subjects and through such a mechanism contributes to differences in disease risk amongst these subjects.
Beta-cell dysfunction in Type 2 diabetes
Once hyperglycaemia exists, beta-cell dysfunction is clearly present in subjects with Type 2 diabetes. This change is manifest in a number of different ways including decreases in the insulin response to intravenous glucose [68, 69, 70] and a decline in the ability of glucose to potentiate the insulin response to non-glucose secretagogues such as the amino acid arginine [71], hormones such as secretin [72], the β-adrenergic agonist isoproterenol [72] and sulfonylureas such as tolbutamide [73]. In addition, alterations in pulsatile insulin release [74, 75] and ultradian oscillatory insulin secretion [76] can be observed. The beta cell is also unable to oscillate in concert with the fluctuations in plasma glucose induced by an oscillating glucose infusion [76]. Finally, inefficient proinsulin processing to insulin [77, 78, 79, 80, 81, 82, 83] and a reduction in the release of islet amyloid polypeptide (IAPP), known also as amylin [84, 85, 86, 87], have been observed in established Type 2 diabetes.
These alterations in beta-cell function have been observed in Type 2 diabetic subjects, typically following the administration of intravenous stimuli. The beta cell's response to oral ingestion, however, involves the simultaneous interaction of a number of functional parameters in order to ensure an insulin response to caloric ingestion. In Type 2 diabetes, assessment of insulin release following oral glucose ingestion has focused both on the early and late plasma insulin responses. Because of the effect of glucose to both stimulate and potentiate the beta cell, insulin concentrations late in the test will frequently appear to be increased compared to those observed in a normal person at the same time point. This observation has led to the concept that beta-cell function in response to oral stimulation may not be deficient in subjects with Type 2 diabetes. However, this conclusion is not correct if the early insulin response (in the first 30 min) is examined. In this case the response is clearly reduced in patients with Type 2 diabetes from a variety of ethnic/race groups and is a definite feature of the disorder [88]. In fact, examination of the data obtained by Yalow and Berson when they developed the insulin RIA clearly demonstrates that patients with early Type 2 diabetes have lost a portion of this early response [89].
Although beta-cell dysfunction is clearly evident in patients with Type 2 diabetes, it is still debated whether this feature is an early abnormality or whether it occurs late in the natural history of the disease. With advances in our understanding of the regulation of insulin release, it seems that beta-cell function is diminished early in the disease process and declines progressively as glucose tolerance deteriorates. This conclusion is based on the understanding that valid representation of beta-cell function requires interpretation of insulin responses in the context of the prevailing degree of insulin sensitivity.
Insulin sensitivity as a modulator of insulin release
Under normal circumstances, insulin secretion by the beta cell is a complex event modulated by a number of variables including the nature and quantity of the secretagogue, the route of its administration, the glucose concentration at the time of administration of the stimulus and the prevailing degree of insulin sensitivity [54, 90]. While the importance of the first four factors has become fairly well understood over the last 25 years or so, the importance of insulin sensitivity as a determinant of the magnitude of the insulin response is less widely appreciated.
From shortly after the development of the insulin RIA, it has been well recognised that obesity and its associated insulin resistance are associated with basal and stimulated hyperinsulinaemia [10, 68, 91, 92]. However, the nature of this regulation was not determined until more recently [54]. With the advent of techniques for quantifying insulin sensitivity, it seems that it is not obesity per se that is responsible for the greater insulin responses but rather that variation in insulin sensitivity modulates insulin release. Thus, insulin-resistant subjects have greater insulin responses to glucose and non-glucose secretagogues whereas insulin-sensitive subjects have smaller insulin responses. We have quantified the relationship between the insulin responses to intravenous stimuli and insulin sensitivity by assessing these two variables in a large cohort of healthy subjects younger than 45 years of age [54]. As postulated previously [93], we found that the relationship between insulin sensitivity and insulin secretion is non-linear and best described by a hyperbolic function. The nature of this relationship implies that the product of insulin sensitivity and insulin response is a constant for a given degree of glucose tolerance. This hyperbolic relationship exists whether the insulin response is examined following intravenous administration of glucose (Fig. 2A) or non-glucose secretagogues (Fig. 2B). Based on these analyses, it is also apparent that the variation in insulin release that occurs in response to differences in insulin sensitivity is the result of changes in the secretory capacity of the beta cell and not its sensitivity to glucose [28, 54] (Fig. 2B). Our finding of a hyperbolic relationship between insulin sensitivity and insulin secretion in healthy subjects has been confirmed in large cohorts of Danish [94] and Pima Indian subjects [95].
The relationship between insulin sensitivity and beta-cell function quantified as (A) the first-phase insulin response (AIRglucose) in 93 (55 men, solid circle; 38 women, open square) apparently healthy, non-diabetic subjects younger than 45 years of age and (B) as the acute insulin response to arginine at maximal glycaemic potentiation (AIRmax) which represents beta-cell secretory capacity in a subset of 43 (27 men, solid circle; 16 women, open square) of these apparently healthy, non-diabetic subjects. The cohort shows a broad range of insulin sensitivity and beta-cell function. The solid line depicts the best-fit relationship (50th percentile) while the broken lines represent the 5th, 25th, 75th and 95th percentiles. The relationship is best described by a hyperbolic function so that any change in insulin sensitivity is balanced by a reciprocal and proportionate change in beta-cell function. Reprinted from [54]
The hyperbola that describes the relationship between insulin sensitivity and insulin release also implies that a feedback loop governs the interaction between the beta cell and the insulin-sensitive tissues. Thus, for glucose tolerance to remain constant when insulin sensitivity varies, a proportionate and reciprocal alteration in insulin output has to occur. This can best be visualised by examining the percentiles for the relationship between insulin sensitivity and the insulin response. The mean relationship is represented as the 50th percentile. Percentiles above the 50th represent enhanced insulin responses for the degree of insulin sensitivity, whereas reduced responses are represented below the 50th percentile (Fig. 2A, B). It would then be predicted that for glucose tolerance to remain constant if insulin sensitivity changes, then the percentile ranking must remain constant. If insulin secretion does not change appropriately, glucose tolerance will differ. Therefore, the product of insulin sensitivity and the insulin response provides a true measure of beta-cell function, rather than the insulin or C-peptide response examined in isolation.
Based on human studies in which an increase or decrease in insulin sensitivity was produced by an experimental intervention, it seems that glucose might not necessarily be the sole mediator of this regulation. This conclusion has been reached based on the fact that the fasting glucose concentration changed in the opposite direction to what would be predicted if it were to be the primary mediator. Thus, the fasting glucose concentration has been observed to increase when insulin sensitivity improved and insulin responses declined [24], a scenario where one would have expected it to be lower. The fasting glucose concentration decreased rather than increased when insulin resistance was produced and insulin release increased as an adaptive response [28]. This adaptive increase in insulin release in response to a decrease in insulin sensitivity can occur relatively quickly, as observed after only 2 weeks of experimental insulin resistance induced by nicotinic acid administration in young healthy subjects [28]. Further validation of the concept of a feedback loop and the need to assess beta-cell function based on the interaction of insulin sensitivity and insulin release is provided by the observation that while insulin secretion increased in response to nicotinic acid-induced insulin resistance, this compensation was incomplete. Thus, the product of insulin sensitivity and the acute insulin response to intravenous glucose, called the disposition index [93], declined in the group as a whole and was associated with a mild deterioration of intravenous glucose tolerance. However, under other circumstances complete adaptation can occur, but this could take longer. As an example, complete adaptation was observed in older subjects who underwent a 6-month intensive exercise training program [24]. In this group, the improvement in insulin sensitivity was balanced by a reciprocal reduction in insulin release resulting in no change in either intravenous or oral glucose tolerance. Thus, the beta cells of older subjects adapted almost perfectly to the increase in insulin sensitivity, "defending" a state of reduced glucose tolerance. Whether this regulation of beta-cell function is governed by a central neural process or is the result of a humoral signal, such as NEFA or one of the incretin peptides, is not known.
The hyperbolic relationship between insulin sensitivity and insulin responses has important implications for estimating the adequacy of a beta-cell response in humans. As differences in insulin sensitivity must be balanced by reciprocal changes in insulin release in order to maintain glucose tolerance, it is apparent that although insulin responses may be identical in groups of subjects, if insulin sensitivity is not the same, beta-cell function is different. Thus, it is essential that we consider insulin sensitivity and insulin responses together when evaluating beta-cell function in subjects at risk of developing Type 2 diabetes and when assessing the importance of beta-cell function to glucose tolerance. These issues, in relation to both intravenous and oral stimulation, are discussed in greater detail in the following two sections.
Beta-cell dysfunction is present prior to the development of Type 2 diabetes: observations with intravenous testing
Data from the UKPDS strongly suggest that beta-cell dysfunction commences years before hyperglycaemia develops [18]. This interpretation is based on a backward extrapolation of findings made in this cohort from shortly after the clinical diagnosis of Type 2 diabetes. Although this concept is certainly gaining support, the need to extrapolate findings from subjects with Type 2 diabetes to that believed to be occurring prior to the diagnosis of the disease is perhaps limiting the acceptance of this idea. Thus, while there is no doubt that defects in beta-cell function exist in all subjects with hyperglycaemia, when this abnormality begins has been a subject of debate. A major reason why there has been a failure to recognise the existence of defects in beta-cell function very early in the course of the development of Type 2 diabetes is because both systems involved in glucose regulation, the islet beta cell and the insulin-sensitive tissues, are commonly not examined in concert.
Based on the concept of a feedback loop, it has become evident that subjects who are at high risk of developing Type 2 diabetes have diminished beta-cell function at a time when many of them still have NGT. Thus, first-degree relatives of patients with Type 2 diabetes [96, 97, 98], women with a history of gestational diabetes [99, 100, 101] or polycystic ovarian disease [96, 102], older subjects [22, 24, 103] and subjects with impaired glucose tolerance [104, 105] can all be shown to have beta-cell dysfunction, manifest as a first-phase insulin response to intravenous glucose that is reduced relative to the degree of insulin sensitivity (Fig. 3). Using this approach, the majority of subjects who have two first-degree relatives with Type 2 diabetes have percentile scores that place them below the mean (50th percentile) for the relationship between insulin sensitivity and insulin secretion, which is in keeping with their high risk status [106] (Fig. 4).
Percentile lines for the relationship between insulin sensitivity (SI) and the first-phase insulin response (AIRglucose) based on data from 93 normal subjects [54]. Mean data from six other studies are plotted. The ten subjects with Type 2 diabetes are insulin-resistant and have markedly impaired insulin secretion [166]. Thirteen healthy older subjects show that aging is associated with insulin resistance and a reduction in beta-cell function [24]. Reduced beta-cell function is also manifest in eight women with a history of gestational diabetes (GDM) [99], 11 women with polycystic ovarian disease (PCO) and a family history of type 2 diabetes [96], 21 subjects with IGT [105], and in 14 subjects with a first-degree relative with type 2 diabetes mellitus [97]. The reduction in beta-cell function in these latter three groups is compatible with their high risk of subsequently developing type 2 diabetes. Reprinted from [167]
Individual values for the percentile scores for the disposition index (SI x AIRg) in 30 first-degree relatives of subjects with Type 2 diabetes and 24 apparently healthy control subjects. The means±SEM for the two groups are illustrated as is the 50th percentile. Amongst the relatives, 21 of the 30 (70%) subjects fall below the 50th percentile whereas in the apparently healthy control subjects 12 out of 24 (50%) do so. The percentile score was determined based on the formula derived in a separate healthy population [54]. Reprinted from [106]
These findings derived from cross-sectional data are supported by a longitudinal study in Pima Indians that has also shown the importance of accounting for the hyperbolic relationship between insulin sensitivity and insulin secretion and demonstrated the presence of impaired beta-cell function in those destined to progress to Type 2 diabetes [95]. Multiple measures of insulin sensitivity and insulin secretion were carried out in subjects in this very high-risk population group who were NGT at baseline and were followed for an average of 5 years (Fig. 5). Seventeen (35%) of these subjects progressed from NGT to IGT and then to diabetes during follow up. At baseline, the NGT subjects who subsequently progressed to hyperglycaemia had an insulin response to glucose that was reduced relative to insulin sensitivity, indicating diminished beta-cell function. During follow up, insulin secretion declined progressively by 78% while insulin sensitivity decreased by only 14%. In a matched group of 31 subjects who did not develop diabetes, insulin sensitivity decreased similarly by 11%, but this change was associated with a 30% increase in insulin secretion, representing an adaptive response to maintain normal beta-cell function. Thus, in this group the expected relationship between insulin sensitivity and insulin release was maintained (Fig. 5).
Changes in beta-cell function measured as the acute insulin response to glucose (AIR) relative to changes in insulin sensitivity measured by the clamp technique at a low insulin concentration (M-low). These measurements were made in 11 Pima Indians in whom glucose tolerance deteriorated from NGT to IGT to diabetes (DIA) (progressors), and in 23 subjects who maintained NGT throughout (non-progressors). The lines represent the prediction line and the lower and upper limits of the 95% confidence interval of the regression between the AIR and M-low as determined from a population of 277 Pima Indians with normal glucose tolerance. Reprinted from [95]
In keeping with the fact that Type 2 diabetes has a strong genetic component, it is of interest that a study examining the heritability of beta-cell function, assessed as the insulin response relative to insulin sensitivity, found a heritability of 67% in 120 subjects who had either IGT or NGT and 70% when only the 94 NGT subjects were examined [107]. When the insulin response to intravenous glucose was considered in isolation, it could not be shown to be an inherited phenotype [107]. This finding suggests that unless the loss of the insulin response is extremely large and already associated with frank diabetes, genetic defects will be difficult to identify unless the modulating effect of insulin sensitivity is considered.
The cross-sectional studies in groups of high risk subjects, the longitudinal study in Pima Indians and the heritability studies in families support the existence of the hyperbolic relationship and the need to interpret beta-cell function based on this interaction. Thus, re-examination of data from some other studies of high risk subjects with NGT would suggest that the conclusions in those papers disputing the presence of beta-cell dysfunction are erroneous because no difference in the insulin responses existed between groups despite the presence of insulin resistance, indicating impaired beta-cell adaptation [108, 109, 110, 111, 112, 113, 114].
Secretion of insulin by the beta cell is typically associated with the release of IAPP. IAPP is co-localized within the same secretory granules as insulin [115] and is typically co-released with insulin in vitro in response to glucose and non-glucose secretagogues [116, 117]. This same parallelism is present in humans in response to both glucose [106, 118] and arginine over a broad range of glucose concentrations [119] with IAPP release being reduced in Type 2 diabetes [84, 85, 86, 87]. Based on the findings of similar insulin and IAPP responses, it could be anticipated that IAPP release would also be modulated by insulin sensitivity. This is indeed the case [120]. Therefore, it could also be predicted that beta-cell function in terms of IAPP release would be diminished in parallel with that of insulin in subjects at risk of developing Type 2 diabetes. We have confirmed this hypothesis in assessments of older subjects and first-degree relatives of subjects with Type 2 diabetes in whom a reduced IAPP response to glucose injection has been shown [106, 118]. As with the insulin response, the magnitude of the IAPP response was similar to that observed in the control groups, the latter comprised of younger subjects and age-matched subjects with no family history respectively. However, as insulin sensitivity was reduced in the subject groups, when the IAPP responses were evaluated in the light of the reduction in insulin sensitivity, the magnitude of the IAPP responses was reduced, representing another manifestation of beta-cell dysfunction. Since the changes in IAPP release were similar to those observed for insulin, it seems that assessing IAPP in high risk subjects does not provide any additional information regarding beta-cell function beyond that obtained by assessing the insulin response relative to the prevailing degree of insulin sensitivity.
These observations examining the early response to intravenous glucose are supported by observations using other intravenous-based tests. Studies in subjects at high risk including first degree relatives of subjects with Type 2 diabetes [121, 122], women with a history of gestational diabetes [100] or polycystic ovarian disease [96] and subjects with IGT [123, 124] have shown reductions in the later (second-phase) insulin response to intravenous glucose [121], in glucose potentiation of insulin release [123], in pulsatile insulin secretion [74, 122], in oscillatory insulin release [96, 100, 124] and in the ability of an oscillating glucose infusion to induce oscillations in insulin secretion [96, 100, 124].
In summary, examination of a number of different intravenous based parameters, especially when considering the prevailing degree of insulin sensitivity, has emphasised the fact that beta-cell dysfunction is present well before the onset of hyperglycaemia. On the other hand, evaluations using data obtained following oral nutrient ingestion are more complex. However, as discussed in the following section, close examination of these responses also shows the presence of impaired beta-cell function in subjects at risk of developing Type 2 diabetes, even when these subjects have NGT.
Beta-cell dysfunction is present prior to the development of Type 2 diabetes: observations with oral testing
After oral glucose ingestion, several factors determine the magnitude of the insulin response [90]. The interpretation of insulin concentrations during an OGTT is complicated by the fact that matching of glucose concentrations and thus the primary stimulus is difficult. This is particularly true later in the test when variation in the glucose concentration also determines the categorisation of glucose tolerance. However, earlier after glucose ingestion, the stimulus presented to the beta cell is more similar and thus the insulin response is more comparable.
In many instances, the early insulin response has been quantified as the increment of the plasma insulin concentration during the first 30 minutes after oral glucose ingestion. To account for the small variations in the magnitude of the glucose stimulus that provokes this early insulin response, it has been divided by the increment in plasma glucose over the same time period [125]. This measurement is frequently referred to as the insulinogenic index. As with intravenous testing, however, this calculated index does not account for the potential modulating and confounding effect of insulin sensitivity on the insulin response.
Because of the severity of the defect, examination of the early insulin response to oral glucose in patients with Type 2 diabetes has shown that this measure is diminished in nearly all populations with the disease. However, in subjects with IGT it has been difficult to consistently demonstrate a reduction in the insulinogenic index, which is even frequently enhanced in this group when compared to those with NGT. On this basis some have ruled out beta-cell dysfunction as a cause of the deterioration in glucose tolerance that defines IGT and concluded that insulin resistance is the primary cause of IGT. Part of the problem could be the appropriate matching of subjects between groups. Indeed, with better matching of subjects for age, sex and obesity, there also does seem to be a decrease of the insulinogenic index in subjects with IGT [5, 87, 88]. This reduction in the early insulin response results in a lack of adequate suppression of hepatic glucose production with subsequent post challenge hyperglycaemia and increased insulin concentrations late in the test [5, 126].
Clearly, it is difficult to match subjects for all the factors that could result in differences in insulin sensitivity if one is to use the insulinogenic index as an appropriate measure of beta-cell function. For example, how can one account for differences in ethnicity, adiposity or body fat distribution that may account for differences in insulin sensitivity and thus the response of the beta cell? One approach is to use a measure of insulin sensitivity and adjust the insulinogenic index appropriately. We have recently performed such an analysis using either the fasting plasma insulin concentration or the HOMA resistance index as a surrogate for the more sophisticated but more complicated measures of insulin sensitivity [88]. The findings obtained with both these surrogate measures of insulin sensitivity were similar.
A total of 531 first-degree relatives of subjects with Type 2 diabetes who themselves had never been diagnosed with diabetes were drawn from four ethnic groups (African American, Asian American, Caucasian and Hispanic American) in the United States [88]. In this large cohort, using recently defined criteria [127], only 45% had NGT with 36% meeting the criteria for IFG and/or IGT and 19% the criteria for diabetes. The four ethnic groups had widely varying degrees of estimated insulin sensitivity even when they had NGT (Fig. 6A). Reductions in glucose tolerance were associated with insulin resistance. Similarly, the early insulin response varied in magnitude in the different groups with NGT and again when glucose tolerance was reduced, this parameter was also reduced (Fig. 6B). When the insulin response was adjusted for the degree of insulin sensitivity, it was apparent that beta-cell function decreased progressively as glucose tolerance deteriorated and that the degree of beta-cell function did not differ by ethnic or racial group for any particular state of glucose tolerance (Fig. 6C). This finding strongly supports the concept that although the magnitude might differ, the factors involved in the pathogenesis of Type 2 diabetes are similar in different ethnic groups and that beta-cell dysfunction is an important contributor.
Insulin sensitivity determined by the HOMA insulin resistance index (A) and beta-cell function quantified as ΔI30/ΔG30 (B) and (ΔI30/ΔG30)/HOMA IR (C) from an OGTT in 531 first-degree relatives of whom 55 were African American (white bar with thin black stripes), 66 Asian American (black bar), 217 Caucasian (dotted bar) and 193 Hispanic American (black bar with thin white stripes). Subjects with IFG or IGT who had diabetes by the 2-h or fasting glucose criteria respectively, were classified as having diabetes. Reprinted from [88]
This large number of subjects with varying degrees of glucose tolerance also provided us an opportunity to examine the contribution of insulin sensitivity and beta-cell function to a measure of glucose disposal after oral glucose ingestion. For these analyses, the efficiency of glucose disposal was assessed as the incremental glucose area under the curve for the 120 min after glucose ingestion. The relationship between insulin sensitivity, quantified as the HOMA resistance index, and glucose disposal was linear in nature but only accounted for 8% of its variance (Fig. 7A). In contrast, the early insulin response was related to glucose disposal in a non-linear manner and accounted for 29% of its variance (Fig. 7B). Beta-cell function, estimated as the insulinogenic index adjusted for insulin sensitivity, was also related to glucose disposal in a non-linear manner and accounted for 45% of its variance (Fig. 7C). The latter relationship indicates that small changes in beta-cell function have rather large effects on glucose disposal in those who already have impaired disposal compared to subjects who have good tolerance. Further analyses of the cohort with NGT and those with IFG or IGT were also very informative (Fig. 8). First, in subjects with NGT who were subdivided into two equal groups each comprising 120 subjects, one with better and the other with poorer glucose disposal, insulin sensitivity did not differ. However, those with the poorer glucose disposal had reduced beta-cell function. Thus, beta-cell function seems to be an important determinant of the variability in glucose disposal in subjects who are considered to have NGT. Second, when glucose metabolism deteriorates and IFG is present, both insulin sensitivity and beta-cell function are diminished suggesting that both abnormalities are simultaneously present in subjects with this more severe derangement in glucose metabolism.
The relationship of insulin sensitivity determined as the HOMA insulin resistance index (A), beta-cell function quantified as ∆I30/∆G30 (B) and as (∆I30/∆G30)/HOMA IR (C) to glucose disposal after an oral glucose load quantified as AUCg in 531 first-degree relatives. The relationship between insulin sensitivity and glucose disposal is linear in nature (r2 = 0.084, p<0.001) while that between beta-cell function and glucose disposal is non-linear and best described by a log-linear fit (∆I30/∆G30: r2=0.29, p<0.001, (∆I30/∆G30)/HOMA IR: r2=0.45, p<0.001). The means for each glucose tolerance category (circle, NGT; diamond, IFG/IGT and square, diabetes) are illustrated. Reprinted from [88]
Insulin sensitivity determined as the HOMA insulin resistance index and beta-cell function quantified as (∆I30/∆G30)/HOMA IR in 240 subjects with NGT divided into two groups (n=120 per group) based on their overall glucose tolerance during an OGTT (A) and in subjects with IGT (n=141) or IFG with or without IGT (n=50) (B). In subjects with NGT, beta-cell function is lower in those with poorer glucose tolerance while insulin sensitivity is not different. In subjects with IFG with or without IGT, both beta-cell function and insulin sensitivity are lower than in those with only IGT. Adapted from [88]
Thus, the findings with the OGTT mirror those made with intravenous testing and strongly suggest that impairments in beta-cell function are present in subjects at high risk of developing Type 2 diabetes, even at a time when they are NGT or IGT. The mechanisms that underlie this change in beta-cell function and contribute to its progressive decline are an area of tremendous research focus.
One factor that we and others have been examining is the deposition of amyloid, which is found in the islets of up to 90% of patients with Type 2 diabetes [128, 129]. These deposits contain IAPP as their unique peptide component [130, 131]. However, the reason(s) why these deposits largely occur in Type 2 diabetes and are not typically observed in subjects with NGT are not clear. The presence of an amyloidogenic amino acid sequence as found in the human peptide is necessary, but on its own is not sufficient [132]. Studies using human IAPP transgenic mice suggest that consumption of increased dietary fat [133] or marked overproduction of IAPP [134, 135] could be important factors in triggering the commencement of islet amyloidogenesis. Work done on non-human primates [136] and transgenic mice [137] support the concept that islet amyloid deposition is an early event in the pathogenesis of Type 2 diabetes being associated with reductions in insulin release well before the onset of hyperglycaemia. In keeping with reduced insulin release in subjects with IGT and Type 2 diabetes after oral glucose ingestion, IAPP release is also progressively reduced in those subjects with impaired glucose metabolism [87]. Thus, it seems that increased IAPP release is not a prerequisite for continued amyloid deposition but rather the continued formation of amyloid is associated with parallel reductions in insulin and IAPP release and reduced beta-cell mass.
Insulin resistance and beta-cell dysfunction: can aspects of their pathogenesis be unified?
The primary metabolic variable glucose, is itself injurious in patients with Type 2 diabetes. This deleterious effect is often referred to as "glucose toxicity" or "glucose desensitization" [138, 139]. The negative impact of glucose has been clearly shown when plasma glucose concentrations reach the range associated with diabetes. In this scenario, glucose lowering is associated with improvements in both insulin sensitivity and insulin release [140]. However, there seems to be a threshold at which this effect is manifest and a pre-existent abnormality is probably needed for glucose to exert a deleterious effect on insulin sensitivity and beta-cell function. This thesis is based on the observation that in apparently healthy subjects the production of hyperglycaemia by a continuous infusion of glucose for periods of up to 42-h is associated with enhancements of insulin sensitivity [141] and beta-cell function [141, 142, 143, 144], rather than the production of insulin resistance and beta-cell dysfunction. These short term studies support the idea that an underlying functional abnormality exists and that the deleterious effects of glucose are an added problem.
The metabolic derangements of Type 2 diabetes include an increase in plasma NEFA concentrations [145], which has been shown to produce deleterious effects on the insulin-sensitive tissues and the beta cell. Exposure to NEFA in vitro decreased insulin-mediated glucose uptake and glycogen synthesis [146] as well as reduced beta-cell function [147, 148], encompassing both reduced insulin release and impaired proinsulin to insulin processing. In vivo, infusion of lipid emulsions and heparin in healthy subjects increased plasma NEFA concentrations to above the physiological range and were associated with the development of insulin resistance, an effect mediated by changes in post-receptor insulin signalling [149, 150, 151]. In response to this reduction in insulin sensitivity, insulin concentrations acutely increase as fatty acids stimulate beta-cell insulin release. Later, insulin concentrations are increased [152], similar [153] or somewhat decreased [154]. However, the lack of an increase in the insulin response is inappropriate in the presence of insulin resistance. Thus, increased NEFA seem to inhibit beta-cell function in vivo. A number of questions remain unanswered from these observations in humans. First, does this relative insulin deficiency represent a true loss of an adaptive response or does adaptation to insulin resistance take longer than the 2 days over which the infusion was administered? Second, if NEFA impair beta-cell function, is an underlying defect essential for the associated reduction in beta-cell function to occur? Third, as with glucose, how does an impairment in the regulation of plasma NEFA concentrations, albeit mild, develop?
A portion of the answer could lie in the early impairment of beta-cell function. The associated reduction in insulin release would be anticipated to result in increased glucose production, reduced efficiency of glucose uptake and increased lipolysis. These aberrations might produce mild increases in plasma glucose and NEFA concentrations. As these substrates increase, they would feed forward in a vicious cycle that begets more insulin resistance and poorer beta-cell function. In addition to its critical role in regulating glucose, lipid and protein metabolism, insulin also has important central nervous system effects, where its action in the hypothalamus reduces food intake and increases energy expenditure [155]. Therefore, a deficiency of insulin action in the brain has the potential to increase body weight, which in turn would diminish insulin sensitivity [156]. Thus, one can envision a beta-cell defect that has a genetic basis and is associated with a reduction in insulin release producing a phenotype of obesity and impaired carbohydrate, lipid and protein metabolism.
Insulin resistance and beta-cell dysfunction: where are we now and what does the future hold?
Today, the importance of both insulin resistance and beta-cell dysfunction in the production of the hyperglycaemia of Type 2 diabetes is apparent. While some may still debate the relative roles of these two parameters, we believe that available data clearly indicate that both are typically present very early in the natural history of the disease. The progressive nature of established Type 2 diabetes is well recognised, and occurs despite attempts to maintain glucose as near to normal as possible [14]. Based on the UKPDS [18] and the longitudinal assessment in Pima Indians [95], the major reason for the decline in glucose tolerance seems to be a progressive loss of beta-cell function. Unfortunately, at this time there is no known pharmacological intervention that is capable of preventing this inexorable decline in beta-cell function in Type 2 diabetic patients.
Recently, a great deal of effort has been made on slowing or even preventing the development of Type 2 diabetes in high risk subjects. In this context, a lifestyle intervention, typically comprising a combination of diet and exercise, reduced the risk of progression from IGT to Type 2 diabetes. This effect was first shown in a feasibility study in Malmö, Sweden [157]. This Swedish study provided the basis for the design of the Da Qing study in China [158], the Finnish Diabetes Prevention Study [159] and the DPP carried out in the United States [16]. All three of these large intervention studies showed a reduction in risk to develop Type 2 diabetes by up to 58% compared to placebo. The mechanisms by which lifestyle changes reduced the rate of development of diabetes in these prevention studies has yet to be reported. However, one can anticipate that the resultant weight loss was associated with improved insulin sensitivity. Further, as a slowing of progression was due to an improvement in glucose tolerance, it is likely that the relationship between insulin sensitivity and insulin secretion changed in accord with an improvement in beta-cell function. However, despite continued intervention, glucose concentrations started to increase again over time. Thus, it seems that a progressive decline in insulin sensitivity and/or beta-cell function was occurring.
While lifestyle changes are clearly beneficial in reducing the risk of developing Type 2 diabetes, they are not practical for all subjects. Thus, medication-based interventions have been and continue to be tested with a number of compounds. In the DPP, metformin was found to be capable of reducing the rate of development of diabetes by 31% relative to placebo [16]. Again, the mechanism by which this effect occurred in subjects with IGT has not yet been reported, but what is apparent is that the compound was more efficacious in terms of modulating the fasting glucose than it was the postprandial glucose. Most recently, the STOP-NIDDM study showed that in subjects with IGT, the α-glucosidase inhibitor acarbose reduced the risk of developing diabetes by 25% [160]. This is interesting because this outcome was achieved with a medication that primarily reduces prandial glucose excursions by slowing glucose absorption from the gastrointestinal tract. Whether the effect of acarbose in this study included indirect effects on insulin sensitivity and beta-cell function, perhaps mediated by the reduction of glycaemia, awaits further analysis. Finally, the TRIPOD study has assessed the effect of troglitazone, a thiazolidinedione, in women with a history of gestational diabetes [161]. This study involved a much smaller cohort and showed that the onset of diabetes could be reduced by 55% with this agent. Furthermore, using sophisticated testing, it was demonstrated that the improvement in insulin sensitivity produced by the medication was associated with an improvement in beta-cell function. Since the DPP initially included a troglitazone treatment arm [162], it will be interesting to learn whether the insulin sensitizer also reduced the risk of developing diabetes in this large diabetes prevention study. Two more large prevention studies examining the effects of the insulin sensitizer rosiglitazone [163] and the beta-cell secretagogue nateglinide [164] have been initiated and should provide further insight into the potential for primary prevention of Type 2 diabetes using approaches that tackle the fundamental defects of the disease prior to the development of clinical hyperglycaemia.
What does the future hold? It is filled with promise, which has to be tempered by the recognition of the magnitude of the problem we face. The broadening of our understanding of the pathophysiology of Type 2 diabetes, in part by the explosion in and continued development of molecular approaches, has moved us forward. It provides the basis for potentially identifying the genetic basis of the disease and for developing new approaches to both the treatment and prevention of Type 2 diabetes. The recent post-hoc analyses showing a possible protective effect on the development of diabetes of the ACE inhibitor ramipril [163] and the HMG CoA reductase inhibitor pravastatin [165] are enticing and emphasise that there are many aspects of the pathogenesis and treatment of the disease that still need to be uncovered.
Sources
This review is based on the relevant literature published in the English language during the period 1990–2001, and seminal prior contributions. The sources available to the author were integrated with sources identified through PubMed searches for "insulin resistance, diabetes and humans" and "insulin secretion, diabetes and humans".
Abbreviations
- DPP:
-
Diabetes Prevention Program
- CT:
-
computed tomography
- HOMA:
-
Homeostasis Model Assessment
- MRI:
-
magnetic resonance imaging
- IAPP:
-
islet amyloid polypeptide
- UKPDS:
-
United Kingdom Prospective Diabetes Study
References
Kahn SE, Porte D, Jr (1996) Pathophysiology of type II diabetes mellitus. In: Porte D Jr, Sherwin RS (eds) Diabetes mellitus. Appleton and Lange, Stamford, pp 487–512
DeFronzo RA, Ferrannini E (1991) Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 14:173–194
Kruszynska YT, Olefsky JM (1996) Cellular and molecular mechanisms of non-insulin dependent diabetes mellitus. J Investig Med 44:413–428
Porte D Jr (1991) β-cells in type II diabetes mellitus. Diabetes 40:166–180
Mitrakou A, Kelley D, Mokan M et al. (1992) Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N Engl J Med 326:22–29
Kahn SE (2001) The importance of beta-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab 86:4047–4058
National Heart Lung and Blood Institute (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. The evidence report. Obes Res 6 [Suppl 2]:51S–209S
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431
Olefsky J, Farquhar JW, Reaven G (1973) Relationship between fasting plasma insulin level and resistance to insulin-mediated glucose uptake in normal and diabetic subjects. Diabetes 22:507–513
Beard JC, Ward WK, Halter JB, Wallum BJ, Porte D Jr (1987) Relationship of islet function to insulin action in human obesity. J Clin Endocrinol Metab 65:59–64
Rosenbloom AL, Joe JR, Young RS, Winter WE (1999) Emerging epidemic of type 2 diabetes in youth. Diabetes Care 22:345–354
Dabelea D, Pettitt DJ, Jones KL, Arslanian SA (1999) Type 2 diabetes mellitus in minority children and adolescents. An emerging problem. Endocrinol Metab Clin North Am 28:709–729
Sinha R, Fisch G, Teague B et al. (2002) Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 346:802–810
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853
Turner RC, Cull CA, Frighi V, Holman RR (1999) Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 281:2005–2012
The Diabetes Prevention Program Research Group (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC (1998) UKPDS 26: Sulphonylurea failure in non-insulin-dependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group. Diabet Med 15:297–303
Holman RR (1998) Assessing the potential for alpha-glucosidase inhibitors in prediabetic states. Diabetes Res Clin Pract 40 [Suppl]:S21-S25
Virkamaki A, Ueki K, Kahn CR (1999) Protein-protein interaction in insulin signaling and the molecular mechanisms of insulin resistance. J Clin Invest 103:931–943
Barroso I, Gurnell M, Crowley VE et al. (1999) Dominant negative mutations in human PPARgamma associated with severe insulin resistance, diabetes mellitus and hypertension. Nature 402:880–883
DeFronzo RA (1979) Glucose intolerance of aging. Evidence for tissue insensitivity to insulin. Diabetes 28:1095–1101
Chen M, Bergman RN, Pacini G, Porte D Jr (1985) Pathogenesis of age-related glucose intolerance in man: insulin resistance and decreased β-cell function. J Clin Endocrinol Metab 60:13–20
Prigeon RL, Kahn SE, Porte D Jr. (1995) Changes in insulin sensitivity, glucose effectiveness, and B-cell function in regularly exercising subjects. Metabolism 44:1259–1263
Kahn SE, Larson VG, Beard JC et al. (1990) Effect of exercise on insulin action, glucose tolerance and insulin secretion in aging. Am J Physiol 258:E937–E943
Chen M, Halter JB, Porte D Jr (1987) The role of dietary carbohydrate in the decreased glucose tolerance of the elderly. J Am Geriatr Soc 35:417–424
Beard JC, Halter JB, Best JD, Pfeifer MA, Porte D Jr (1984) Dexamethasone-induced insulin resistance enhances B-cell responsiveness to glucose level in normal men. Am J Physiol 247:E592–E596
Rizza RA, Mandarino LJ, Gerich JE (1982) Effects of growth hormone on insulin action in man. Mechanisms of insulin resistance, impaired suppression of glucose production, and impaired stimulation of glucose utilization. Diabetes 31:663–669
Kahn SE, Beard JC, Schwartz MW et al. (1989) Increased β-cell secretory capacity as mechanism for islet adaptation to nicotinic acid-induced insulin resistance. Diabetes 38:562–568
Kolterman OG, Insel J, Saekow M, Olefsky JM (1980) Mechanisms of insulin resistance in human obesity: evidence for receptor and postreceptor defects. J Clin Invest 65:1272–1284
Lillioja S, Bogardus C (1988) Obesity and insulin resistance: lessons learned from the Pima Indians. Diabetes Metab Rev 4:517–540
Bjorntorp P (1993) Visceral obesity: a "civilization syndrome". Obes Res 1:206–222
Peiris AN, Mueller RA, Smith GA, Struve MF, Kissebah AH (1986) Splanchnic insulin metabolism in obesity. Influence of body fat distribution. J Clin Invest 78:1648–1657
Pouliot MC, Despres JP, Nadeau A et al. (1992) Visceral obesity in men. Associations with glucose tolerance, plasma insulin, and lipoprotein levels. Diabetes 41:826–834
Peiris AN, Sothmann MS, Hennes MI et al. (1989) Relative contribution of obesity and body fat distribution to alterations in glucose insulin homeostasis: predictive values of selected indices in premenopausal women. Am J Clin Nutr 49:758–764
Fujimoto WY, Abbate SL, Kahn SE, Hokanson JE, Brunzell JD (1994) The visceral adiposity syndrome in Japanese-American men. Obes Res 2:364–371
Abate N, Garg A, Peshock RM, Stray-Gundersen J, Grundy SM (1995) Relationships of generalized and regional adiposity to insulin sensitivity in men. J Clin Invest 96:88–98
Goodpaster BH, Kelley DE, Wing RR, Meier A, Thaete FL (1999) Effects of weight loss on regional fat distribution and insulin sensitivity in obesity. Diabetes 48:839–847
Cnop M, Landchild MJ, Vidal J et al. (2002) The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations: distinct metabolic effects of two fat compartments. Diabetes 51:1005–1015
Taylor SI, Cama A, Accili D et al. (1992) Mutations in the insulin receptor gene. Endocr Rev 13:566–595
Xia J, Scherer SW, Cohen PT et al. (1998) A common variant in PPP1R3 associated with insulin resistance and type 2 diabetes. Diabetes 47:1519–1524
Hegele RA, Harris SB, Zinman B et al. (1998) Variation in the AU(AT)-rich element within the 3′-untranslated region of PPP1R3 is associated with variation in plasma glucose in aboriginal Canadians. J Clin Endocrinol Metab 83:3980–3983
Hansen L, Hansen T, Vestergaard H et al. (1995) A widespread amino acid polymorphism at codon 905 of the glycogen-associated regulatory subunit of protein phosphatase-1 is associated with insulin resistance and hypersecretion of insulin. Hum Mol Genet 4:1313–1320
Hansen L, Reneland R, Berglund L et al. (2000) Polymorphism in the glycogen-associated regulatory subunit of type 1 protein phosphatase (PPP1R3) gene and insulin sensitivity. Diabetes 49:298–301
Stumvoll M, Tschritter O, Fritsche A et al. (2002) Association of the T-G polymorphism in adiponectin (exon 2) with obesity and insulin sensitivity: interaction with family history of type 2 diabetes. Diabetes 51:37–41
Hasstedt SJ, Ren QF, Teng K, Elbein SC (2001) Effect of the peroxisome proliferator-activated receptor-gamma 2 pro(12)ala variant on obesity, glucose homeostasis, and blood pressure in members of familial type 2 diabetic kindreds. J Clin Endocrinol Metab 86:536–541
Deeb SS, Fajas L, Nemoto M et al. (1998) A Pro12Ala substitution in PPARgamma2 associated with decreased receptor activity, lower body mass index and improved insulin sensitivity. Nat Genet 20:284–287
Altshuler D, Hirschhorn JN, Klannemark M et al. (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80
Horton ES (1986) Exercise and physical training: effects on insulin sensitivity and glucose metabolism. Diabetes Metab Rev 2:1–17
Chen M, Bergman RN, Porte D Jr (1988) Insulin resistance and β-cell dysfunction in aging: the importance of dietary carbohydrate. J Clin Endocrinol Metab 67:951–957
Brunzell JD, Lerner RL, Hazzard WR, Porte D Jr, Bierman EL (1971) Improved glucose tolerance with high carbohydrate feeding in mild diabetes. N Engl J Med 284:521–524
Despres JP, Moorjani S, Lupien PJ, Tremblay A, Nadeau A, Bouchard C (1990) Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 10:497–511
Peiris AN, Sothmann MS, Hoffmann RG et al. (1989) Adiposity, fat distribution, and cardiovascular risk. Ann Intern Med 110:867–872
Abate N, Garg A, Peshock RM, Stray-Gundersen J, Adams-Huet B, Grundy SM (1996) Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes 45:1684–1693
Kahn SE, Prigeon RL, McCulloch DK et al. (1993) Quantification of the relationship between insulin sensitivity and B-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Cnop M, Havel PJ, Utzschneider KM et al. (2002) Gender-based differences in adiponectin and leptin levels are related to differences in body fat distribution. Diabetes 50 [Suppl 2]:A404 (Abstract)
Matsuzawa Y, Funahashi T, Nakamura T (1999) Molecular mechanism of metabolic syndrome X: contribution of adipocytokines adipocyte-derived bioactive substances. Ann NY Acad Sci 892:146–154
Weyer C, Funahashi T, Tanaka S et al. (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 86:1930–1935
Hotta K, Funahashi T, Arita Y et al. (2000) Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol 20:1595–1599
Couillard C, Mauriege P, Prud'homme D et al. (1997) Plasma leptin concentrations: gender differences and associations with metabolic risk factors for cardiovascular disease. Diabetologia 40:1178–1184
Schwartz RS, Shuman WP, Bradbury VL et al. (1990) Body fat distribution in healthy young and older men. J Gerontol 45:M181-M185
Purnell JQ, Kahn SE, Albers JJ, Nevin DN, Brunzell JD, Schwartz RS (2000) Effect of weight loss with reduction of intra-abdominal fat on lipid metabolism in older men. J Clin Endocrinol Metab 85:977–982
Schwartz RS, Shuman WP, Larson V et al. (1991) The effect of intensive endurance exercise training on body fat distribution in young and older men. Metabolism 40:545–551
Auwerx J (1999) PPARgamma, the ultimate thrifty gene. Diabetologia 42:1033–1049
Hirose H, Kawai T, Yamamoto Y et al. (2002) Effects of pioglitazone on metabolic parameters, body fat distribution, and serum adiponectin levels in Japanese male patients with type 2 diabetes. Metabolism 51:314–317
Mori Y, Murakawa Y, Okada K et al. (1999) Effect of troglitazone on body fat distribution in type 2 diabetic patients. Diabetes Care 22:908–912
Steppan CM, Bailey ST, Bhat S et al. (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312
Yang WS, Jeng CY, Wu TJ et al. (2002) Synthetic peroxisome proliferator-activated receptor-gamma agonist, rosiglitazone, increases plasma levels of adiponectin in type 2 diabetic patients. Diabetes Care 25:376–380
Perley MJ, Kipnis DM (1967) Plasma insulin responses to oral and intravenous glucose: studies in normal and diabetic subjects. J Clin Invest 46:1954–1962
Bagdade JD, Bierman EL, Porte D Jr (1967) The significance of basal insulin levels in the evaluation of the insulin response to glucose in diabetic and nondiabetic subjects. J Clin Invest 46:1549–1557
Brunzell JD, Robertson RP, Lerner RL et al. (1976) Relationships between fasting plasma glucose levels and insulin secretion during intravenous glucose tolerance tests. J Clin Endocrinol Metab 42:222–229
Ward WK, Bolgiano DC, McKnight B, Halter JB, Porte D Jr (1984) Diminished B cell secretory capacity in patients with noninsulin-dependent diabetes mellitus. J Clin Invest 74:1318–1328
Halter JB, Porte D Jr (1978) Mechanisms of impaired acute insulin release in adult onset diabetes: studies with isoproterenol and secretin. J Clin Endocrinol Metab 46:952–960
Varsano-Aharon N, Echemendia E, Yalow RS, Berson SA (1970) Early insulin responses to glucose and to tolbutamide in maturity-onset diabetes. Metabolism 19:409–417
O'Rahilly S, Turner RC, Matthews DR (1988) Impaired pulsatile secretion of insulin in relatives of patients with non-insulin-dependent diabetes. N Engl J Med 318:1225–1230
Porksen N (2002) The in vivo regulation of pulsatile insulin secretion. Diabetologia 45:3–20
Polonsky KS, Given BD, Hirsch LJ et al. (1988) Abnormal patterns of insulin secretion in non-insulin-dependent diabetes mellitus. N Engl J Med 318:1231–1239
Mako ME, Starr JI, Rubenstein AH (1977) Circulating proinsulin in patients with maturity-onset diabetes. Am J Med 63:865–869
Ward WK, LaCava EC, Paquette TL, Beard JC, Wallum BJ, Porte D Jr (1987) Disproportionate elevation of immunoreactive proinsulin in type 2 (non-insulin-dependent) diabetes mellitus and experimental insulin resistance. Diabetologia 30:698–702
Yoshioka N, Kuzuya T, Matsuda A, Taniguchi M, Iwamoto Y (1988) Serum proinsulin levels at fasting and after oral glucose load in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 31:355–360
Temple RC, Clark PM, Nagi DK, Schneider AE, Yudkin JS, Hales CN (1990) Radioimmunoassay may overestimate insulin in non-insulin-dependent diabetics. Clin Endocrinol (Oxf) 32:689–693
Saad MF, Kahn SE, Nelson RG et al. (1990) Disproportionately elevated proinsulin in Pima Indians with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 70:1247–1253
Kahn SE, Leonetti DL, Prigeon RL, Bergstrom RW, Fujimoto WY (1995) Relationship of proinsulin and insulin with noninsulin-dependent diabetes mellitus and coronary heart disease in Japanese American men: impact of obesity. J Clin Endocrinol Metab 80:1399–1406
Kahn SE, Halban PA (1997) Release of incompletely processed proinsulin is the cause of the disproportionate proinsulinemia of NIDDM. Diabetes 46:1725–1732
Sanke T, Hanabusa T, Nakano Y et al. (1991) Plasma islet amyloid polypeptide (amylin) levels and their responses to oral glucose in type 2 (non-insulin-dependent) diabetic patients. Diabetologia 34:129–132
Ludvik B, Lell B, Hartter E, Schnack C, Prager R (1991) Decrease of stimulated amylin release precedes impairment of insulin secretion in type II diabetes. Diabetes 40:1615–1619
Enoki S, Mitsukawa T, Takemura J et al. (1992) Plasma islet amyloid polypeptide levels in obesity, impaired glucose tolerance and non-insulin-dependent diabetes mellitus. Diabetes Res Clin Pract 15:97–102
Kahn SE, Verchere CB, Andrikopoulos S et al. (1998) Reduced amylin release is a characteristic of impaired glucose tolerance and type 2 diabetes in Japanese Americans. Diabetes 47:640–645
Jensen CC, Cnop M, Hull RL, Fujimoto WY, Kahn SE, American Diabetes Association GENNID Study Group (2002) β-cell function is the major determinant of oral glucose tolerance in four ethnic groups in the United States. Diabetes 51:2170–2178
Yalow RS, Berson SA (1960) Plasma insulin concentrations in nondiabetic and early diabetic subjects: determinations by a new sensitive immunoassay technic. Diabetes 9:254–260
Ward WK, Beard JC, Halter JB, Pfeifer MA, Porte D Jr (1984) Pathophysiology of insulin secretion in non-insulin-dependent diabetes mellitus. Diabetes Care 7:491–502
Karam JH, Grodsky GM, Forsham PH (1963) Excessive insulin response to glucose in obese subjects as measured by immunochemical assay. Diabetes 12:197–204
Bagdade JD, Porte D Jr, Brunzell JD, Bierman EL (1974) Basal and stimulated hyperinsulinism: reversible metabolic sequelae of obesity. J Lab Clin Med 83:563–569
Bergman RN, Phillips LS, Cobelli C (1981) Physiologic evaluation of factors controlling glucose tolerance in man: measurement of insulin sensitivity and β-cell glucose sensitivity from the response to intravenous glucose. J Clin Invest 68:1456–1467
Clausen JO, Borch-Johnsen K, Ibsen H et al. (1996) Insulin sensitivity index, acute insulin response, and glucose effectiveness in a population-based sample of 380 young healthy Caucasians. Analysis of the impact of gender, body fat, physical fitness, and life-style factors. J Clin Invest 98:1195–1209
Weyer C, Bogardus C, Mott DM, Pratley RE (1999) The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest 104:787–794
Ehrmann DA, Sturis J, Byrne MM, Karrison T, Rosenfield RL, Polonsky KS (1995) Insulin secretory defects in polycystic ovary syndrome. Relationship to insulin sensitivity and family history of non-insulin-dependent diabetes mellitus. J Clin Invest 96:520–527
Kahn SE (1996) Regulation of B-cell function in vivo: from health to disease. Diabetes Rev 4:372–389
Elbein SC, Wegner K, Kahn SE (2000) Reduced β-cell compensation to the insulin resistance associated with obesity in members of Caucasian familial type 2 diabetic kindreds. Diabetes Care 23:221–227
Ward WK, Johnston CLW, Beard JC, Benedetti TJ, Halter JB, Porte D Jr (1985) Insulin resistance and impaired insulin secretion in subjects with histories of gestational diabetes mellitus. Diabetes 34:861–869
Ryan EA, Imes S, Liu D et al. (1995) Defects in insulin secretion and action in women with a history of gestational diabetes. Diabetes 44:506–512
Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK (1999) Antepartum predictors of the development of type 2 diabetes in Latino women 11–26 months after pregnancies complicated by gestational diabetes. Diabetes 48:2430–2436
Dunaif A, Finegood DT (1996) Beta-cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome. J Clin Endocrinol Metab 81:942–947
Kahn SE, Larson VG, Schwartz RS et al. (1992) Exercise training delineates the importance of B-cell dysfunction to the glucose intolerance of human aging. J Clin Endocrinol Metab 74:1336–1342
Larsson H, Ahren B (1996) Islet dysfunction in obese women with impaired glucose tolerance. Metabolism 45:502–509
Cavaghan MK, Ehrmann DA, Byrne MM, Polonsky KS (1997) Treatment with the oral antidiabetic agent troglitazone improves beta cell responses to glucose in subjects with impaired glucose tolerance. J Clin Invest 100:530–537
Knowles NG, Landchild MA, Fujimoto WY, Kahn SE (2002) Insulin and amylin release are both diminished in first-degree relatives of subjects with type 2 diabetes. Diabetes Care 25:292–297
Elbein SC, Hasstedt SJ, Wegner K, Kahn SE (1999) Heritability of pancreatic beta-cell function among nondiabetic members of Caucasian familial type 2 diabetic kindreds. J Clin Endocrinol Metab 84:1398–1403
Haffner S, Stern M, Hazuda H, Mitchell B, Patterson J (1988) Increased insulin concentrations in nondiabetic offspring of diabetic parents. N Engl J Med 319:1297–1301
Lillioja S, Mott DM, Howard BV et al. (1988) Impaired glucose tolerance as a disorder of insulin action. Longitudinal and cross-sectional studies in Pima Indians. N Engl J Med 318:1217–1225
Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Intern Med 113:909–915
Martin BL, Warram JH, Krolewski AS, Bergman RN, Soeldner JS, Kahn CR (1992) Role of glucose and insulin resistance in development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet 340:925–929
Eriksson J, Franssila Kallunki A, Ekstrand A et al. (1989) Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus. N Engl J Med 321:337–343
Lillioja S, Mott DM, Spraul M et al. (1993) Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. Prospective studies of Pima Indians. N Engl J Med 329:1988–1992
Ferrannini E (1998) Insulin resistance versus insulin deficiency in non-insulin-dependent diabetes mellitus: problems and prospects. Endocr Rev 19:477–490
Lukinius A, Wilander E, Westermark GT, Engstrom U, Westermark P (1989) Co-localization of islet amyloid polypeptide and insulin in the B cell secretory granules of the human pancreatic islets. Diabetologia 32:240–244
Kahn SE, D'Alessio DA, Schwartz MW et al. (1990) Evidence of cosecretion of islet amyloid polypeptide and insulin by β-cells. Diabetes 39:634–638
Kahn SE, Fujimoto WY, D'Alessio DA, Ensinck JW, Porte D Jr (1991) Glucose stimulates and potentiates islet amyloid polypeptide secretion by the B-cell. Horm Metab Res 23:577–580
Dechenes CJ, Verchere CB, Andrikopoulos S, Kahn SE (1998) Human aging is associated with parallel reductions in insulin and amylin release. Am J Physiol 275:E785–E791
Larsson H, Ahren B (1995) Effects of arginine on the secretion of insulin and islet amyloid polypeptide in humans. Pancreas 11:201–205
Landchild MJ, Knowles NG, Yao Q et al. (2000) Increased β-cell secretory demand is not the simple explanation for inefficient proinsulin processing and islet amyloid formation in type 2 diabetes. J Investig Med 48:21A (Abstract)
Pimenta W, Korytkowski M, Mitrakou A et al. (1995) Pancreatic beta-cell dysfunction as the primary genetic lesion in NIDDM. Evidence from studies in normal glucose-tolerant individuals with a first-degree NIDDM relative. JAMA 273:1855–1861
Schmitz O, Porksen N, Nyholm B et al. (1997) Disorderly and nonstationary insulin secretion in relatives of patients with NIDDM. Am J Physiol 272:E218–E226
Larsson H, Ahren B (1996) Failure to adequately adapt reduced insulin sensitivity with increased insulin secretion in women with impaired glucose tolerance. Diabetologia 39:1099–1107
O'Meara NM, Sturis J, Van Cauter E, Polonsky KS (1993) Lack of control by glucose of ultradian insulin secretory oscillations in impaired glucose tolerance and in non-insulin-dependent diabetes mellitus. J Clin Invest 92:262–271
Phillips DI, Clark PM, Hales CN, Osmond C (1994) Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med 11:286–292
Kelley D, Mokan M, Veneman T (1994) Impaired postprandial glucose utilization in non-insulin-dependent diabetes mellitus. Metabolism 43:1549–1557
American Diabetes Association (1997) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20:1183–1197
Clark A, Saad MF, Nezzer T et al. (1990) Islet amyloid polypeptide in diabetic and non-diabetic Pima Indians. Diabetologia 33:285–289
Kahn SE, Andrikopoulos S, Verchere CB (1999) Islet amyloid: a long-recognized but underappreciated pathological feature of type 2 diabetes. Diabetes 48:241–253
Westermark P, Wernstedt C, Wilander E, Hayden DW, O'Brien TD, Johnson KH (1987) Amyloid fibrils in human insulinoma and islets of Langerhans of the diabetic cat are derived from a neuropeptide-like protein also present in normal islets. Proc Natl Acad Sci USA 84:3881–3885
Cooper GJS, Willis AC, Clark A, Turner RC, Sim RB, Reid KBM (1987) Purification and characterization of a peptide from amyloid-rich pancreases of type 2 diabetic patients. Proc Natl Acad Sci USA 84:8628–8632
Westermark P, Engstrom U, Johnson KH, Westermark GT, Betsholtz C (1990) Islet amyloid polypeptide: pinpointing amino acid residues linked to amyloid fibril formation. Proc Natl Acad Sci USA 87:5036–5040
Verchere CB, D'Alessio DA, Palmiter RD et al. (1996) Islet amyloid formation associated with hyperglycemia in transgenic mice with pancreatic beta cell expression of human islet amyloid polypeptide. Proc Natl Acad Sci USA 93:3492–3496
Soeller WC, Janson J, Hart SE et al. (1998) Islet amyloid-associated diabetes in obese Avy/a mice expressing human islet amyloid polypeptide. Diabetes 47:743–750
Höppener JW, Oosterwijk C, Nieuwenhuis MG et al. (1999) Extensive islet amyloid formation is induced by development of Type II diabetes mellitus and contributes to its progression: pathogenesis of diabetes in a mouse model. Diabetologia 42:427–434
Howard CF Jr (1986) Longitudinal studies on the development of diabetes in individual Macaca nigra. Diabetologia 29:301–306
Wang F, Hull RL, Vidal J, Cnop M, Kahn SE (2001) Islet amyloid develops diffusely throughout the pancreas before becoming severe and replacing endocrine cells. Diabetes 50:2514–2520
Yki-Järvinen H (1992) Glucose toxicity. Endocr Rev 13:415–431
Robertson RP, Olson LK, Zhang HJ (1994) Differentiating glucose toxicity from glucose desensitization: a new message from the insulin gene. Diabetes 43:1085–1089
Garvey WT, Olefsky JM, Griffen J, Hamman RF, Kolterman OG (1985) The effect of insulin treatment on insulin secretion and insulin action in type II diabetes mellitus. Diabetes 34:222–234
Kahn SE, Bergman RN, Schwartz MW, Taborsky GJ Jr, Porte D Jr (1992) Short-term hyperglycemia and hyperinsulinemia improve insulin action but do not alter glucose action in normal humans. Am J Physiol 262:E518–E523
Ward WK, Halter JB, Beard JC, Porte D Jr (1984) Adaptation of B and A cell function during prolonged glucose infusion in human subjects. Am J Physiol 246:E405–E411
Byrne MM, Sturis J, Polonsky KS (1995) Insulin secretion and clearance during low-dose graded glucose infusion. Am J Physiol 268:E21–E27
Hartling SG, Røder ME, Dinesen B, Binder C (1996) Proinsulin, C-peptide, and insulin in normal subjects during an 8-h hyperglycemic clamp. Eur J Endocrinol 134:197–200
Reaven GM, Hollenbeck C, Jeng CY, Wu MS, Chen YD (1988) Measurement of plasma glucose, free fatty acid, lactate, and insulin for 24 h in patients with NIDDM. Diabetes 37:1020–1024
Thompson AL, Lim-Fraser MY, Kraegen EW, Cooney GJ (2000) Effects of individual fatty acids on glucose uptake and glycogen synthesis in soleus muscle in vitro. Am J Physiol Endocrinol Metab 279:E577-E584
Zhou YP, Grill VE (1994) Long-term exposure of rat pancreatic islets to fatty acids inhibits glucose-induced insulin secretion and biosynthesis through a glucose fatty acid cycle. J Clin Invest 93:870–876
Zhou YP, Grill V (1995) Long term exposure to fatty acids and ketones inhibits B-cell functions in human pancreatic islets of Langerhans. J Clin Endocrinol Metab 80:1584–1590
Boden G (1997) Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes 46:3–10
Roden M, Price TB, Perseghin G et al. (1996) Mechanism of free fatty acid-induced insulin resistance in humans. J Clin Invest 97:2859–2865
Griffin ME, Marcucci MJ, Cline GW et al. (1999) Free fatty acid-induced insulin resistance is associated with activation of protein kinase C theta and alterations in the insulin signaling cascade. Diabetes 48:1270–1274
Boden G, Chen X, Rosner J, Barton M (1995) Effects of a 48-h fat infusion on insulin secretion and glucose utilization. Diabetes 44:1239–1242
Carpentier A, Mittelman SD, Lamarche B, Bergman RN, Giacca A, Lewis GF (1999) Acute enhancement of insulin secretion by FFA in humans is lost with prolonged FFA elevation. Am J Physiol 276:E1055–E1066
Paolisso G, Gambardella A, Amato L et al. (1995) Opposite effects of short- and long-term fatty acid infusion on insulin secretion in healthy subjects. Diabetologia 38:1295–1299
Schwartz MW, Woods SC, Porte D Jr, Seeley RJ, Baskin DG (2000) Central nervous system control of food intake. Nature 404:661–671
Porte D Jr, Seeley RJ, Woods SC, Baskin DG, Figlewicz DP, Schwartz MW (1998) Obesity, diabetes and the central nervous system. Diabetologia 41:863–881
Eriksson K-F, Lindgarde F (1991) Prevention of Type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise: the 6-year Malmo: feasibility study. Diabetologia 34:891–898
Pan XR, Li GW, Hu YH et al. (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 20:537–544
Tuomilehto J, Lindstrom J, Eriksson JG et al. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M (2002) Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 359:2072–2077
Buchanan TA, Xiang AH, Peters RK et al. (2002) Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high- risk hispanic women. Diabetes 51:2796–2803
The Diabetes Prevention Program Research Group (1999) The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 22:623–634
Yusuf S, Gerstein H, Hoogwerf B et al. (2001) Ramipril and the development of diabetes. JAMA 286:1882–1885
Haffner S, Holman R, Califf R, McMurray J, Pehcer E (2002) Targeting post-prandial hyperglycemia to prevent type 2 diabetes: Rationale and design of the NAVIGATOR trial. Diabetologia 45 [Suppl 2]:A106 (Abstract)
Freeman DJ, Norrie J, Sattar N et al. (2001) Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation 103:357–362
Welch S, Gebhart SSP, Bergman RN, Phillips LS (1990) Minimal model analysis of intravenous glucose tolerance test-derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab 71:1508–1518
Vidal J, Kahn SE (2001) Regulation of insulin secretion in vivo. In: Lowe WL Jr (ed.) Genetics of Diabetes Mellitus. Kluwer, Stamford, pp 109–131
Acknowledgements
This work was supported by the Medical Research Service of the Department of Veterans Affairs and by NIH grants DK-02654, DK-17047, DK-50703 and RR-37.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kahn, S.E. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 46, 3–19 (2003). https://doi.org/10.1007/s00125-002-1009-0
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-002-1009-0